End of life care for infants, children and young people with life limiting conditions: summary of NICE guidance
BMJ 2016; 355 doi: https://doi.org/10.1136/bmj.i6385 (Published 08 December 2016) Cite this as: BMJ 2016;355:i6385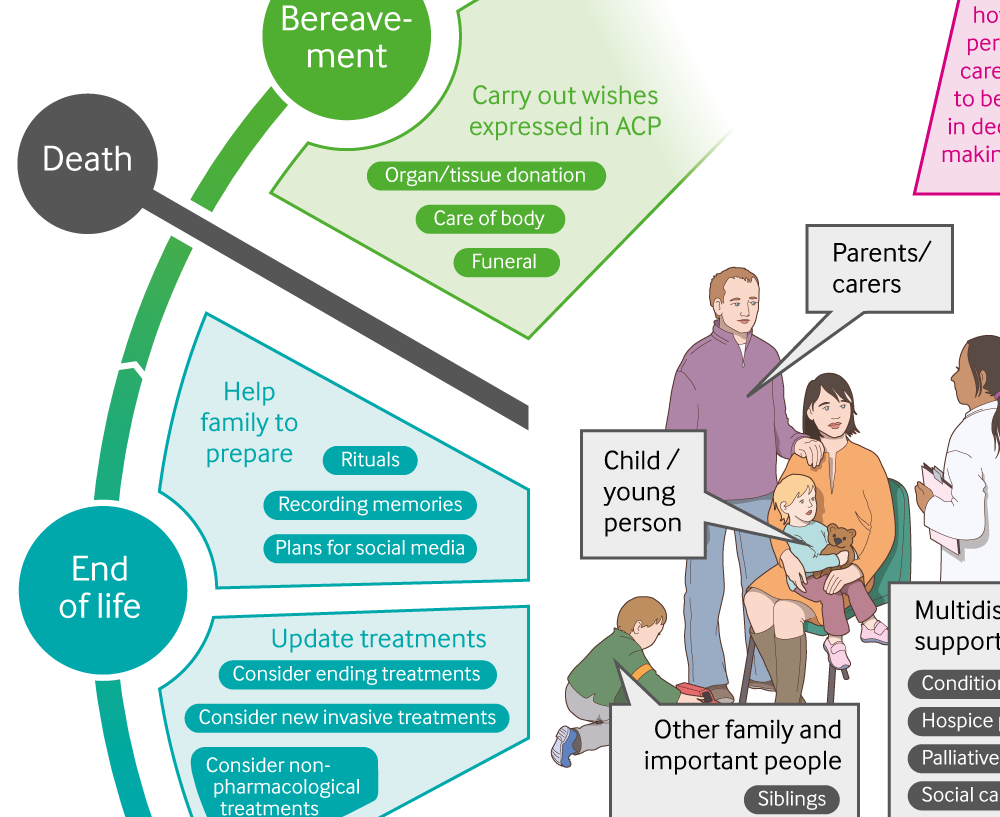
Infographic available
Click here for a visual summary of the recommendations for end of life care for children and young people, including likely needs of young person and their family, professional involvement required, and advance care planning.

Chinese translation
该文章的中文翻译
- Gemma Villanueva, senior systematic reviewer1,
- M Stephen Murphy, clinical advisor1,
- David Vickers, chair of guideline committee, consultant paediatrician and medical director2 3,
- Emily Harrop, deputy chair of the guideline committee, consultant in paediatric palliative care4 5,
- Katharina Dworzynski, guideline lead1
- 1National Guideline Alliance, Royal College of Gynaecologists and Obstetricians, London NW1 4RG, UK
- 2Cambridgeshire Community Services NHS Trust, St Ives PE27 4LG, UK
- 3East Anglia’s Children's Hospices, Milton CB24 6DF, UK
- 4Helen & Douglas House, Oxford OX4 1RW, UK
- 5Oxford University Hospitals, Oxford OX3 9DU, UK
- Correspondence to: K Dworzynski kdworzynski{at}rcog.org.uk
What you need to know
Involve children and young people with life limiting conditions and their parents or carers in decision making and care planning
An advance care plan is a core element of a child’s or young person’s end of life care
Be aware that other family members such as siblings and grandparents, and others (such as friends, boyfriends or girlfriends) may need support
Name a medical specialist who leads on and coordinates the child or young person’s care
Decisions about care should always consider what it is the best interest of the child
Children and young people can have a wide range of life limiting conditions and may sometimes live with such conditions for many years. This guideline recommends that end of life care be managed as a long term process that begins at the time of diagnosis of a life limiting condition and entails planning for the future. Sometimes it may begin before the child’s birth. It is part of the overall care of the child or young person and runs in parallel with other active treatments for the underlying condition itself.1 Finally, it includes those aspects related to the care of the dying.
This guideline was commissioned with the aim to standardise end of life care for infants, children, and young people living with a life limiting condition, and thus promote equity and consistency. Important themes are to involve children and young people and their parents or carers in decisions about their care, facilitate their care in their preferred location (most likely home), and plan for day and night care.
This article summarises the most recent guidance from the recent National Institute for Health and Care Excellence (NICE) on the planning and management of end of life care in infants, children, and young people.2 For a visual summary, please see infographic.
Recommendations
NICE recommendations are based on systematic reviews of the best available evidence, although this was often of low or at best moderate quality, and explicit consideration of cost effectiveness. When minimal evidence is available, recommendations are based on the Guideline Committee’s (GC) experience and opinion of what constitutes good practice. Evidence levels for the recommendations are given in italic in square brackets.
How to plan care
Recognise that children and young people with life limiting conditions and their parents or carers have a central role in decision making and care planning. [Based on very low to moderate quality evidence from qualitative studies and the experience and opinion of the Guideline Committee (GC)]
Explain to children and young people and to their parents or carers that their contribution to decisions about their care is important, but they do not have to make decisions alone and the multidisciplinary team will be involved as well. [Based on moderate to very low quality evidence from qualitative studies and the experience and opinion of the GC]
Advanced care planning
Develop and record an advance care plan at an appropriate time for the current and future care of each child or young person with a life limiting condition (see box 1). [Based on very low to moderate quality evidence from qualitative studies and the experience and opinion of the GC]
In some cases planning may begin antenatally.
Box 1: Components of an advance care plan for a child or young person with a life limiting condition
Demographic information about the child or young person and their family
Up to date contact information for:
The child or young person’s parents or carers
The key professionals involved in care
A statement about who has responsibility for giving consent
A summary of the life limiting condition
An agreed approach to communicating with and providing information to the child or young person and their parents or carers
An outline of the child or young person's life ambitions and wishes, such as on:
Family and other relationships
Social activities and participation
Education
How to incorporate their religious, spiritual, and cultural beliefs and values into their care
A record of significant discussions with the child or young person and their parents or carers
Agreed treatment plans and objectives
Education plans, if relevant
A record of any discussions and decisions that have taken place on:
Preferred place of care and place of death
Organ and tissue donation (see recommendation 1.1.19 in the full NICE guideline2)
Management of life threatening events, including plans for resuscitation or life support
Specific wishes, such as on funeral arrangements and care of the body
A distribution list for the advance care plan
[Based on the experience and opinion of the GC]
Share the advance care plan with the child or young person and their parents or carers (as appropriate), and think about which professionals and services involved in the individual child or young person’s care should also share it, for example:
General practitioners
Hospital consultants
Hospices
Respite centres
Nursing services (community or specialist)
School and other education services
Ambulance services.
[Based on very low to moderate quality evidence from qualitative studies and the experience and opinion of the GC]
Multidisciplinary team working
Depending on the needs of the child or young person, the multidisciplinary team may include:
Healthcare professionals from primary, secondary, or tertiary services, including with specialists in the child’s underlying life limiting condition, hospice professionals, and members of the specialist palliative care team (see recommendation 1.5.4 in the full NICE guideline2)
Social care practitioners
Education professionals
Chaplains
Allied health professionals (such as physiotherapists, occupational therapists, and psychological therapists).
[Based on the experience and opinion of the GC]
Every child or young person with a life limiting condition should have a named medical specialist who leads on and coordinates their care. Explain to the child or young person and their parents or carers that their named medical specialist may change if the care that is needed or the care setting changes. [Based on the experience and opinion of the GC]
Emotional and psychological support
Regularly discuss emotional and psychological wellbeing with children and young people and their parents or carers, particularly at times of change such as:
When the life limiting condition is diagnosed
If their clinical condition deteriorates
If their personal circumstances change
If there are changes to their nursery care, school, or college arrangements, or their employment
If there are changes to their clinical care (for example, if their care changes focus from treating the condition to end of life care).
[Based on the experience and opinion of the GC]
Social and practical support
Be aware that other family members (such as grandparents) and people important to the child or young person (such as friends, boyfriends or girlfriends) may need support, including social, practical, emotional, psychological, and spiritual support. [Based on the experience and opinion of the GC]
Be aware that siblings will need support to cope with:
Their brother’s or sister’s condition and death
The effects of their parents’ or carers’ grieving.
[Based on the experience and opinion of the GC]
Be aware that children and young people with life limiting conditions and their parents or carers have varied social and practical support needs, and that those needs may change during the course of their condition. This may include:
Material support, such as housing or adaptations to the home and equipment for home drug infusions
Practical support, such as access to respite care
Technical support, such as training and help with administering drug infusions at home
Education support, such as from hospital school services
Financial support.
[Based on very low to moderate quality evidence from qualitative studies and the experience and opinion of the GC]
Approaching the end of life
When a child or young person is approaching the end of life, discuss with their parents or carers what would help them, for example:
Important rituals
Recording or preserving memories (for example, photographs, hair locks, or hand prints)
Plans for social media content.
[Based on very low to moderate quality evidence from qualitative studies and the experience and opinion of the GC]
Agree the preferred place of care and place of death with children and young people and their parents or carers, taking into account:
Their wishes, which are personal and individual
Their religious, spiritual, and cultural values
The views of relevant and experienced healthcare professionals
Safety and practicality.
[Based on the experience and opinion of the GC]
Explain that the place of care or place of death may change, for example:
If the child or young person and their parents or carers change their minds or
For clinical reasons or
Due to problems with service provision.
[Based on very low quality evidence from qualitative studies and the experience and opinion of the GC]
For children and young people with life limiting conditions who are approaching the end of life and are being cared for at home, services should provide (when needed):
Advice from a consultant in paediatric palliative care (such as by telephone) at any time (day and night)
Paediatric nursing care at any time
Home visits by a healthcare professional from the specialist paediatric palliative care team (see recommendation 1.5.4 in the full NICE guideline2), for example, for symptom management
Practical support and equipment for interventions including oxygen, enteral nutrition, and subcutaneous and intravenous therapies
Anticipatory prescribing for children and young people who are likely to develop symptoms.
[Based on the experience and opinion of the GC]
Involve the specialist paediatric palliative care team if a child or young person has unresolved distressing symptoms as they approach the end of life. [Based on the experience and opinion of the GC]
Think about non-pharmacological interventions for pain management, such as:
Changes that may help them to relax, for example, environmental adjustments (for example reducing noise), music or physical contact (such as touch, holding or massage)
Local hot or cold applications to the site of pain
Comfort measures, such as sucrose for neonates.
[Based on the experience and opinion of the GC]
Titrate treatment to provide continuous background analgesia, and prescribe additional doses for breakthrough pain if this occurs.
In addition to background analgesia, consider giving anticipatory doses of analgesia for children and young people who have pain at predictable times (for example, when changing dressings or moving and handling). Do not include anticipatory doses when calculating the required daily background dose of analgesia. [Based on the experience and opinion of the GC]
When a child or young person is approaching the end of life, discuss with them and their parents or carers and with relevant healthcare professionals:
Any available invasive treatments that might be in their best interest
Any interventions they are currently receiving that may no longer be in their best interest.
[Based on the experience and opinion of the GC]
Attempt resuscitation for children and young people with life limiting conditions unless there is a “Do not attempt resuscitation” order in place. [Based on the experience and opinion of the GC]
Education into practice
Has an advance care plan been developed and recorded, when appropriate, for the children and young people with a life limiting condition in your care?
Are there services in place that can provide round the clock care for a child or young person with a life limiting condition who is approaching the end of life?
Can patients and their families be cared for in their preferred place of care?
Are children or young people with life limiting conditions receiving symptom management that is adequate to maximise their quality of life?
How patients were involved in the creation of this article
Patients were not directly involved in this article. Committee members involved in this guideline included two patient representatives, who contributed to the formulation of the recommendations summarised here. Children and young people with life limiting conditions also contributed to this guideline by having their voices heard by focus groups.
Further information on the guidance
Methods
This guidance was developed by the National Guideline Alliance in accordance with NICE guideline development methods (www.nice.org.uk/media/default/about/what-we-do/our-programmes/developing-nice-guidelines-the-manual.pdf).
A Guideline Committee (GC) was established by the National Guideline Alliance, which incorporated healthcare and allied healthcare professionals (one consultant in neonatal medicine, one neonatologist, two consultant paediatricians, one consultant paediatric intensivist, one consultant in paediatric palliative care, one honorary consultant, one general practitioner, two nurse consultants, one clinical nurse specialist, one clinical psychologist, one children and families worker, one youth worker, one ethicist, and one chaplain) and two lay members. The GC co-opted a pharmacist, a specialist nurse in organ donation, and a bereavement support coordinator.
The GC identified relevant clinical questions, collected and appraised clinical evidence, and evaluated the cost effectiveness of proposed interventions where possible. Qualitative reviews were undertaken to explore aspects related to information and communication, support, and advance care planning.
Quality ratings of the evidence were based on GRADE methodology (www.gradeworkinggroup.org/). These relate to the quality of the available evidence for assessed outcomes or themes rather than the quality of the study.
Focus groups with children and young people with life limiting conditions were conducted for this guideline. The findings of this research were used as direct evidence to inform recommendations. This work was carried out by Together for Short Lives, an organisation representing the needs of children and young people with life limiting conditions.
The scope and the draft of the guideline went through a rigorous reviewing process, in which stakeholder organisations were invited to comment; the group took all comments into consideration when producing the final version of the guideline.
Three different versions of this guideline have been produced: a full version containing all the evidence, the process undertaken to develop the recommendations, and all the recommendations, known as the “full guideline”; a short version containing a list of all the recommendations, known as the “short guideline”; and a version on the information for patients product, known as the “information for the public guideline.” All of these versions are available from the NICE website (www.nice.org.uk/guidance/NG61).
A formal review of the need to update a guideline is usually undertaken by NICE after its publication. NICE will conduct a review to determine whether the evidence base has progressed significantly to alter the guideline recommendations and warrants an update.
Future research
The GC prioritised the following research recommendations:
When planning and managing end of life care, what factors help children and young people with life limiting conditions and their parents or carers decide where they would like end of life care to be provided and where they prefer to die?
What is the impact of offering timely perinatal palliative care on the experience of bereaved families? What emotional support do children and young people with life limiting conditions and their parents or carers need, and how would they like these needs to be addressed?
What are the acceptability, safety, and effectiveness of different types of opioid analgesia for breakthrough pain in children and young people with life limiting conditions who are having end of life care in the community?
What signs and symptoms indicate that a child or young person with a life limiting condition is likely to die within hours or days?
Footnotes
The members of the Guideline Committee were Amy Volans, Bobbie Farsides, Claire Wansley, David Vickers (chair), Elissa Coster (until September 2015), Emily Harrop (deputy chair from April 2016), Fauzia Paize (from May 2015), Jane Green, Karen Brombley, Lucy Coombes, Paul Nash, Peter Barry, Satbir Jassal, Sharon English (until March 2015), Stacey Curzon (from November 2015), and Zoe Picton-Howell. Co-opted members were Afia Manaf, David Hamilton, and Susan Lee.
The members of the National Guideline Alliance technical team were Alexandra Hellyer (from March 2016 to August 2016), Gemma Villanueva (from March 2015), Jessica Sims (until December 2014), Kate Coles (from December 2014 to March 2015), Katharina Dworzynski (from March 2015), Paul Jacklin, Rishiraj Caleyachetty (from December 2014 to March 2015), Sabrina Naqvi (from August 2016), Stephen Murphy, Timothy Reeves, and Yelan Guo.
Contributors: All authors contributed to the initial draft of this article, helped revise the manuscript, and approved the final version for publication.
Funding: The National Guideline Alliance was commissioned and funded by the National Institute for Health and Care Excellence to develop this guideline and write this BMJ summary.
Competing interests: We declare the following interests based on NICE's policy on conflicts of interests (available at www.nice.org.uk/Media/Default/About/Who-we-are/Policies-and-procedures/code-of-practice-for-declaring-and-managing-conflicts-of-interest.pdf): authors’ full statements can be viewed at www.bmj.com/content/bmj/355/bmj.i6385/related#datasupp.
