Abstract
Background:
The Neonatal Intensive Care Unit (NICU) can be ethically charged, which can create challenges for health-care workers.
Objective:
To determine the frequency with which nurses and residents have experienced ethical confrontations and what factors are associated with increased frequency.
Design/Methods:
An anonymous questionnaire was distributed to nurses in a university center, a high-risk obstetric service, a maternity hospital NICU with 85% in-born patients and an outborn NICU, most of whose preterm admissions are those with surgical complications. Obstetric and pediatric residents in the four universities of the province also received the questionnaire, which included demographics, opinions regarding the gestational age threshold at which resuscitation of a premature infant with bradycardia was appropriate, knowledge of cerebral palsy (CP) outcomes (as an indicator of knowledge about long-term sequelae of prematurity) and questions about ethical confrontation in the NICU.
Results:
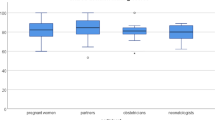
Two hundred and seventy-nine caregivers participated (115 full time nurses and 164 residents). All the distributed questionnaires were completed. Frequent ethical confrontation was reported by 35% of the nurses and 19% of the residents. Among the nurses, moral distress differed significantly between work environments. Nurses working in an out-born NICU and obstetric nurses were more likely to overestimate CP prevalence (P<0.05). Nurses who overestimated CP rates had higher thresholds for resuscitation and were more likely to experience ethical confrontations. Of the residents, 60% were pediatric and 40% obstetric. All groups of residents frequently overestimated the prevalence of CP, and knowledge differed significantly by residency program (P<0.05). The residents who overestimated CP rates had higher thresholds for resuscitation, had more incorrect answers regarding prematurity outcomes and were less likely to have ethical confrontations.
Conclusions:
A large proportion of nurses and residents report frequent ethical confrontations. Many residents and nurses have limited knowledge of outcomes and high threshold for resuscitation. Ethical confrontation is more common among nurses with poor knowledge about outcomes, and less common in residents with poor knowledge about outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Austin W, Lemermeyer G, Goldberg L, Bergum V, Johnson MS . Moral distress in healthcare practice: the situation of nurses. HEC Forum 2005; 17(1): 33–48.
Partridge JC, Martinez AM, Nishida H, Boo N-Y, Tan KW, Yeung C-Y et al. International comparison of care for very low birth weight infants: parents' perceptions of counseling and decision-making. Pediatrics 2005; 116(2): e263–e271.
De Leeuw R, Cuttini M, Nadai M, Berbik I, Hansen G, Kucinskas A et al. Treatment choices for extremely preterm infants: an international perspective. J Pediatr 2000; 137(5): 608–616.
Blanco F, Suresh G, Howard D, Soll RF . Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics 2005; 115(4): e478–e487.
Lee SK, Penner PL, Cox M . Comparison of the attitudes of health care professionals and parents toward active treatment of very low birth weight infants. Pediatrics 1991; 88(1): 110–114.
Haywood JL, Morse SB, Goldenberg RL, Bronstein J, Nelson KG, Carlo WA . Estimation of outcome and restriction of interventions in neonates. Pediatrics 1998; 102(2): E201–E205.
Morse SB, Haywood JL, Goldenberg RL, Bronstein J, Nelson KG, Carlo WA . Estimation of neonatal outcome and perinatal therapy use. Pediatrics 2000; 105(5): 1046–1050.
Lefebvre F, Mazurier E, Tessier R . Cognitive and educational outcomes in early adulthood for infants weighing 1000 g or less at birth. Acta Paediatr 2005; 94(6): 733–740.
Teplin SW, Burchinal M . Neurodevelopmental, health, and growth status at age 6 years of children with birth weights less than 1001 g. J Pediatr 1991; 118: 768.
Saigal S, Rosenbaum P, Hattersley B, Milner R . Decreased disability rate among 3-year-old survivors weighing 501 to 1000 g at birth and born to residents of a geographically defined region from 1981 to 1984 compared with 1977 to 1980. J Pediatr 1989; 114: 839–846.
Wilkinson JM . Moral distress: a labor and delivery nurse's experience. J Obstet Gynecol Neonatal Nurs 1989; 18(6): 513–519.
Hefferman P, Heilig S . Giving ‘moral distress’ a voice: ethical concerns among neonatal intensive care unit personnel. Camb Q Healthc Ethics 1999; 8(2): 173–178.
Tiedje LB . Moral distress in perinatal nursing. J Perinat Neonatal Nurs 2000; 14(2): 36–43.
Hakansson S, Farooqi A, Holmgren PA, Serenius F, Hogberg U . Proactive management promotes outcome in extremely preterm infants: a population-based comparison of two perinatal management strategies. Pediatrics 2004; 114(1): 58–64.
Saigal S, Rosenbaum PL, Feeny D, Burrows E, Furlong W, Stoskopf BL et al. Parental perspectives of the health status and health-related quality of life of teen-aged children who were extremely low birth weight and term controls. Pediatrics 2000; 105(3 Part 1): 569–574.
Elpern EH, Covert B, Kleinpell R . Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care 2005; 14(6): 523–530.
Solomon MZ, Sellers DE, Heller KS, Dokken DL, Levetown M, Rushton C et al. New and lingering controversies in pediatric end-of-life care. Pediatrics 2005; 116(4): 872–883.
Corley MC, Minick P, Elswick RK, Jacobs M . Nurse moral distress and ethical work environment. Nurs Ethics 2005; 12(4): 381–390.
Meltzer LS, Huckabay LM . Critical care nurses' perceptions of futile care and its effect on burnout. Am J Crit Care 2004; 13(3): 202–208.
Cronqvist A, Lutzen K, Nystrom M . Nurses' lived experiences of moral stress support in the intensive care context. J Nurs Manage 2006; 14(5): 405–413.
Acknowledgements
There is no financial support to report, and no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Janvier, A., Nadeau, S., Deschênes, M. et al. Moral distress in the neonatal intensive care unit: caregiver's experience. J Perinatol 27, 203–208 (2007). https://doi.org/10.1038/sj.jp.7211658
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211658
Keywords
This article is cited by
-
A systematic scoping review moral distress amongst medical students
BMC Medical Education (2022)
-
Developing a digitally innovative ethics and professionalism curriculum for neonatal-perinatal medicine fellows: a 3-year multicenter pilot study
Journal of Perinatology (2022)
-
Exploring implicit bias in the perceived consequences of prematurity amongst health care providers in North Queensland – a constructivist grounded theory study
BMC Pregnancy and Childbirth (2021)
-
Moral distress in the neonatal intensive care unit: an Italian study
Journal of Perinatology (2015)
-
End-of-life care in a regional level IV neonatal intensive care unit after implementation of a palliative care initiative
Journal of Perinatology (2015)