Abstract
Objective:
To evaluate the efficacy of prophylactic antibiotics in preventing infection associated with central venous catheters in preterm neonates.
Study Design:
The search strategy of the Cochrane Neonatal Review Group was used. The following databases were searched: Medline, Cochrane Central Register of Controlled Trials, CINAHL and EMBASE. In addition, we hand-searched abstracts of Pediatric Academic Societies annual meetings published in Pediatric Research (1990 to July 2007) and Canadian Pediatric Society annual meeting proceedings (1990 to July 2007). No language restrictions were applied. Included were randomized controlled trials of antibiotics given prophylactically to prevent infection in preterm infants (<37 completed weeks) less than 1-month old admitted to neonatal intensive care units. Both centrally or peripherally inserted central venous catheters were included. Assessment of methodological quality and extraction of data for included trials was undertaken independently by two authors. When suitable, data from trials were combined in a meta-analysis.
Result:
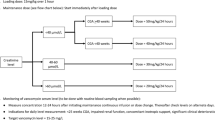
A total of three studies were found which addressed the role of prophylactic antibiotics to prevent catheter-related infection in neonates. Two studies used vancomycin as the prophylactic antibiotic and one study used amoxicillin. The meta-analysis of studies that used vancomycin had shown an absolute risk reduction of infection from 23 to 2.4%, which yields a number needed to treat equal to 5 (P=0.0001). Total duration of catheter stay and mortality, were both similar in the vancomycin and control groups. In the amoxicillin study, catheter-related sepsis was not significantly different between the treatment and control groups (P=0.40). The rate of colonization, however, was significantly higher in the control group (relative risk 0.48; 95% CI 0.12, 1.35). The incidence of necrotizing enterocolitis, intracranial hemorrhage, thrombosis and deaths were not statistically significant between groups.
Conclusion:
Prophylactic vancomycin appeared to be effective in preventing catheter-related sepsis in preterm neonates. The potential risks, however, of the emergence of resistance because of prophylactic antibiotics, and their continued effectiveness, need further evaluation, before routine use can be recommended.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chien LY, Macnab Y, Aziz K, Andrews W, McMillan DD, Lee SK . Variations in central venous catheter-related infection risks among Canadian neonatal intensive care units. Pediatr Infect Dis J 2002; 21 (6): 505–511.
Freeman J, Epstein MF, Smith NE, Platt R, Sidebottom DG, Goldmann DA . Extra hospital stay and antibiotic usage with nosocomial coagulase-negative staphylococcal bacteremia in two neonatal intensive care unit populations. Am J Dis Child 1990; 144 (3): 324–329.
Garland JS, Buck RK, Maloney P, Durkin DM, Toth-Lloyd S, Duffy M et al. Comparison of 10% povidone-iodine and 0.5% chlorhexidine gluconate for the prevention of peripheral intravenous catheter colonization in neonates: a prospective trial. Pediatr Infect Dis J 1995; 14 (6): 510–516.
Grisoni ER, Mehta SK, Connors AF . Thrombosis and infection complicating central venous catheterization in neonates. J Pediatr Surg 1986; 21 (9): 772–776.
Salzman MB, Isenberg HD, Shapiro JF, Lipsitz PJ, Rubin LG . A prospective study of the catheter hub as the portal of entry for microorganisms causing catheter-related sepsis in neonates. J Infect Dis 1993; 167 (2): 487–490.
Schiff DE, Stonestreet BS . Central venous catheters in low birth weight infants: incidence of related complications. J Perinatol 1993; 13 (2): 153–158.
Aly H, Herson V, Duncan A, Herr J, Bender J, Patel K et al. Is bloodstream infection preventable among premature infants? A tale of two cities. Pediatrics 2005; 115 (6): 1513–1518.
Brooker RW, Keenan WJ . Catheter related bloodstream infection following PICC removal in preterm infants. J Perinatol 2007; 27 (3): 171–174.
Harris MC, Polin RA . Neonatal septicemia. Pediatr Clin North Am 1983; 30 (2): 243–258.
St Geme III JW, Polin RA . Neonatal sepsis. Progress in diagnosis and management. Drugs 1988; 36 (6): 784–800.
Ainsworth SB, Clerihew L, McGuire W . Percutaneous central venous catheters versus peripheral cannulae for delivery of parenteral nutrition in neonates. Cochrane Database Syst Rev 2004; (2): CD004219.
Hall SL . Coagulase-negative staphylococcal infections in neonates. Pediatr Infect Dis J 1991; 10 (1): 57–67.
Maki DG, Cobb L, Garman JK, Shapiro JM, Ringer M, Helgerson RB . An attachable silver-impregnated cuff for prevention of infection with central venous catheters: a prospective randomized multicenter trial. Am J Med 1988; 85 (3): 307–314.
Maki DG, Ringer M . Evaluation of dressing regimens for prevention of infection with peripheral intravenous catheters. Gauze, a transparent polyurethane dressing, and an iodophor-transparent dressing. JAMA 1987; 258 (17): 2396–2403.
Snydman DR, Gorbea HF, Pober BR, Majka JA, Murray SA, Perry LK . Predictive value of surveillance skin cultures in total-parenteral-nutrition-related infection. Lancet 1982; 2 (8312): 1385–1388.
Craft A, Finer N . Nosocomial coagulase negative staphylococcal (CoNS) catheter-related sepsis in preterm infants: definition, diagnosis, prophylaxis, and prevention. J Perinatol 2001; 21 (3): 186–192.
van Tulder M, Furlan A, Bombardier C, Bouter L . Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine 2003; 28 (12): 1290–1299.
Garland JS, Alex CP, Henrickson KJ, McAuliffe TL, Maki DG . A vancomycin–heparin lock solution for prevention of nosocomial bloodstream infection in critically ill neonates with peripherally inserted central venous catheters: a prospective, randomized trial. Pediatrics 2005; 116 (2): e198–e205.
Harms K, Herting E, Kron M, Schiffmann H, Schulz-Ehlbeck H . Randomized, controlled trial of amoxicillin prophylaxis for prevention of catheter-related infections in newborn infants with central venous silicone elastomer catheters. J Pediatr 1995; 127 (4): 615–619.
Spafford PS, Sinkin RA, Cox C, Reubens L, Powell KR . Prevention of central venous catheter-related coagulase-negative staphylococcal sepsis in neonates. J Pediatr 1994; 125 (2): 259–263.
Barefield ES, Philips III JB . Vancomycin prophylaxis for coagulase-negative staphylococcal bacteremia. J Pediatr 1994; 125 (2): 230–232.
Eichelberger MR, Rous PG, Hoelzer DJ, Garcia VF, Koop CE . Percutaneous subclavian venous catheters in neonates and children. J Pediatr Surg 1981; 16 (4 Suppl 1): 547–553.
Fallat ME, Gallinaro RN, Stover BH, Wilkerson S, Goldsmith LJ . Central venous catheter bloodstream infections in the neonatal intensive care unit. J Pediatr Surg 1998; 33 (9): 1383–1387.
Munson DP, Thompson TR, Johnson DE, Rhame FS, VanDrunen N, Ferrieri P . Coagulase-negative staphylococcal septicemia: experience in a newborn intensive care unit. J Pediatr 1982; 101 (4): 602–605.
Ogata ES, Schulman S, Raffensperger J, Luck S, Rusnak M . Caval catheterization in the intensive care nursery: a useful means for providing parenteral nutrition to the extremely low birth-weight infant. J Pediatr Surg 1984; 19 (3): 258–262.
Warner BW, Gorgone P, Schilling S, Farrell M, Ghory MJ . Multiple purpose central venous access in infants less than 1000 g. J Pediatr Surg 1987; 22 (9): 820–822.
Henrickson KJ, Axtell RA, Hoover SM, Kuhn SM, Pritchett J, Kehl SC et al. Prevention of central venous catheter-related infections and thrombotic events in immunocompromised children by the use of vancomycin/ciprofloxacin/heparin flush solution: a randomized, multicenter, double-blind trial. J Clin Oncol 2000; 18 (6): 1269–1278.
Safdar N, Maki DG . Use of vancomycin-containing lock or flush solutions for prevention of bloodstream infection associated with central venous access devices: a meta-analysis of prospective, randomized trials. Clin Infect Dis 2006; 43 (4): 474–484.
Mermel LA . Prevention of intravascular catheter-related infections. Ann Intern Med 2000; 132 (5): 391–402.
Acknowledgements
We thank Ms Elizabeth Uleryk, Hospital Library and Archives, The Hospital for Sick Children and University of Toronto, Toronto and Ms Denise Upton, Health Sciences Library, University of Calgary, Calgary, Canada for their contribution in developing the search strategy and for conducting parts of the literature search. Ms Uleryk and Ms Upton received no financial compensation for this support. This study was not supported by any funding. Abhay Lodha developed the original protocol, conducted the search strategies, performed quality assessments/data extraction and wrote the final paper. Andrea D Furlan developed the original protocol, conducted the search strategies, performed quality assessments/data extraction and wrote the final paper. Hilary Whyte contributed to all aspect of the review from start to completion. Aideen M Moore contributed to all aspect of the review from start to completion.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimers: Nil.
Rights and permissions
About this article
Cite this article
Lodha, A., Furlan, A., Whyte, H. et al. Prophylactic antibiotics in the prevention of catheter-associated bloodstream bacterial infection in preterm neonates: a systematic review. J Perinatol 28, 526–533 (2008). https://doi.org/10.1038/jp.2008.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.31
This article is cited by
-
Epidemiology and risk factors for thrombosis in children and newborns: systematic evaluation and meta-analysis
BMC Pediatrics (2023)
-
Prävention von Gefäßkatheter-assoziierten Infektionen bei Früh- und Neugeborenen
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2018)
-
Prevention of neonatal late-onset sepsis: a randomised controlled trial
BMC Pediatrics (2017)
-
Peripherally inserted central venous catheters: frequency of complications in premature newborn depends on the insertion site
Journal of Perinatology (2014)
-
Nosokomiale Sepsis bei sehr kleinen Frühgeborenen
Monatsschrift Kinderheilkunde (2014)