Abstract
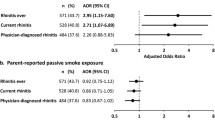
Due to impaired airway function, children are at risk for adverse respiratory symptoms if exposed to environmental tobacco smoke (ETS). A community-based, cross-sectional study of 425 children (5–11 years) attending 15 primary schools in a low socio-economic area of Merseyside/UK was undertaken to investigate the association of adverse respiratory symptoms and ETS exposure using a parent-completed questionnaire and children’s salivary cotinine measurements. Overall, 28.9% of children had doctor-diagnosed asthma (DDA) and 11.3% a history of hospital admission for respiratory illnesses. The symptom triad of cough, wheeze and breathlessness (C+W+B+) occurred in 12.6% of children. The geometric mean cotinine level was 0.37 ng/ml (95% CI, 0.33–0.42 ng/ml) and it was estimated that 45.6% of children were ETS exposed. A history of asthma in the family was reported for 9.2% of fathers and 7.2% of mothers. Salivary cotinine level was significantly increased in children with DDA compared to those without (P = 0.002). Cotinine-validated levels [adjusted odds ratio (AOR), 1.8; 95% CI, 1.4–2.5), low socio-economic (disadvantaged) status (AOR, 1.4; 1.1–2.9), child’s male gender (AOR, 1.6; 1.1–2.5) and maternal smoking (AOR, 2.2; 1.4–3.1) were significantly associated with DDA. The cotinine-validated level (AOR, 1.4; 1.1–2.9) as well as maternal smoking (AOR, 1.8; 1.1–2.5), were also independently associated with C+W+B+. The use of salivary cotinine as an indicator of ETS exposure could be used to inform parents of exposure risk to their asthmatic children and may help re-enforce deterrent efforts to reduce childhood parental smoking exposure.


Similar content being viewed by others
References
David, G. L., Koh, W. P., Lee, H. P., Yu, M. C., & London, S. J. (2005). Childhood exposure to environmental tobacco smoke and chronic respiratory symptoms in non-smoking adults: The Singapore Chinese Health Study. Thorax, 60(12), 1052–1058.
Delpisheh, A., Brabin, L., & Brabin, B. J. (2006). Pregnancy, smoking and birth outcomes. Women’s Health, 2(3), 389–403.
Brabin, B., Smith, M., Milligan, P., Benjamin, C., Dunne, E., & Pearson, M. (1994). Respiratory morbidity in Merseyside schoolchildren exposed to coal dust and air pollution. Archives of Disease in Childhood, 70(4), 305–312.
Berz, J. B., Carter, A. S., Wagmiller, R. L., Horwitz, S. M., Murdock, K. K., & Briggs-Gowan, M. (2007). Prevalence and correlates of early onset asthma and wheezing in a healthy birth cohort of 2- to 3-year olds. Journal of Pediatric Psychology, 32(2), 154–166.
Law, M., Morris, J. K., Watt, H. C., & Wald, N. J. (1997). The dose-response relationship between cigarette consumption, biochemical markers and risk of lung cancer. British Journal of Cancer, 75(11), 1690–1693.
Jones, S. (2004). The need to protect children from second-hand tobacco smoke. Professional Nurse, 19(5), 285.
Karadag, B., Karakoc, F., Ceran, O., Ersu, R., Inan, S., & Dagli, E. (2003). Does passive smoke exposure trigger acute asthma attack in children? Allergologia et Immunopatholia (Madr), 31(6), 318–323.
Jarvis, M., Goddard, E., Higgins, V., Feyerabend, C., Bryant, A., & Cook, D. G. (2000). Children’s exposure to passive smoking in England since the 1980s: Cotinine evidence from population surveys. British Medical Journal, 321(7257), 343–345.
Phillips, K., Bentley, M. C., Abrar, M., Howar, D. A., & Cook, J. (1999). Low level saliva cotinine determination and its application as a biomarker for environmental tobacco smoke exposure. Human & Experimental Toxicology, 18(4), 291–296.
Delpisheh, A., Topping, J., Reyad, M., Tang, A., & Brabin, B. J. (2007). Smoking exposure in pregnancy: Use of salivary cotinine in monitoring. British Journal of Midwifery, 15(4), 216–220.
Bernaards, C. M., Twisk, J. W., van Mechelen, W., Snel, J., & Kemper, H. C. (2004). Comparison between self-report and a dipstick method (NicCheck 1) to assess nicotine intake. European Addiction Research, 10(4), 163–167.
Child, F., Lenney, W., Clayton, S., Davies, S., Jones, P. W., Alldersea, J. E., et al. (2003) The association of maternal but not paternal genetic variation in GSTP1 with asthma phenotypes in children. Respiratory Medicine, 97(12), 1247–1256.
Carroll, W. D., Lenney, W., Child, F., Strange, R. C., Jones, P. W., & Fryer, A. A. (2005). Maternal glutathione S-transferase GSTP1 genotype is a specific predictor of phenotype in children with asthma. Pediatric Allergy and Immunology, 16(1), 32–39.
Young, S., Sherrill, D. L., Arnott, J., Diepeveen, D., LeSouef, P. N., & Landau, L. I. (2000). Parental factors affecting respiratory function during the first year of life. Pediatric Pulmonology, 29(5), 331–340.
Almqvist, C., Pershagen, G., & Wickman, M. (2005). Low socioeconomic status as a risk factor for asthma, rhinitis and sensitization at 4 years in a birth cohort. Clinical and Experimental Allergy, 35(5), 612–618.
Rizwan, S., Reid, J., Kelly, Y., Bundred, P. E., Pearson, M., & Brabin, B. J. (2004). Trends in childhood and parental asthma prevalence in Merseyside, 1991–1998. Journal of Public Health (Oxford), 26(4), 337–342.
Clifford, R. D., Radford, M., Howell, J. B., & Holgate, S. T. (1989). Prevalence of respiratory symptoms among 7 and 11 year old schoolchildren and association with asthma. Archives of Disease in Childhood, 64(8), 1118–1125.
Delpisheh, A., Kelly, Y., & Brabin, B. J. (2006). Passive cigarette smoke exposure in primary school children in Liverpool. Public Health, 120(1), 65–69.
Bland, J. M., & Altman, D. G. (1986). Statistical methods for assessing agreement between two methods of clinical measurement. Lancet, 1(8476), 307–10.
Townsend, P., Phillimore, P., & Saracci, R. (1988). Health and deprivation, inequality and the north. London: Croom Helm.
Delpisheh, A., Kelly, Y., Rizwan, S., & Brabin, B. J. (2006). Socio-economic status, smoking during pregnancy and birth outcomes: An analysis of cross-sectional community studies in Liverpool (1993–2001). Journal of Child Health Care, 10(2), 140–148.
Burr, M., Anderson, H. R., Austin, J., Harkins, L., & Strachan, D. (1999). Respiratory symptoms and home environment in children: A national survey. Thorax, 54(4), 27–32.
Kelly, Y. J., Brabin, B. J., Milligan, P. J., Reid, J. A., Heaf, D., & Pearson, M. G. (1996). Clinical significance of cough and wheeze in the diagnosis of asthma. Archives of Disease in Childhood, 75(6), 489–493.
Goncalves-Silva, R. M., Valente, J. G., Lemos-Santos, M. G., & Sichieri, R. (2006). Household smoking and respiratory disease in under-five children. Cadernos de saude publica, 22(3), 579–586.
Austin, J. B., Selvaraj, S., Godden, D., & Russell, G. (2005). Deprivation, smoking, and quality of life in asthma. Archives of Disease in Childhood, 90(3), 253–7.
Li, H., Romieu, I., Sienra-Monge, J. J., Ramirez-Aguilar, M., Estela Del Rio-Navarro, B., & Kistner, E. O., et al. (2006). Genetic polymorphisms in arginase I and II and childhood asthma and atopy. The Journal of Allergy and Clinical Immunology, 117(1), 119–126.
Girodet, P. O., Casset, A., Magnan, A., de Blay, F., Chanez, P., & Tunon De Lara, J. M. (2005). IgE and respiratory disease. Revue des Maladies Respiratoires, 22(6 Pt 1), 967–981.
Kabesch, M. (2006). Gene by environment interactions and the development of asthma and allergy. Toxicology Letters, 162(1), 43–48.
Li, Y. F., Gilliland, F. D., Berhane, K., McConnell, R., Gauderman, W. J., Rappaport, E. B., et al. (2000). Effects of in utero and environmental tobacco smoke exposure on lung function in boys and girls with and without asthma. American Journal of Respiratory and Critical Care Medicine, 162(6), 2097–2104.
Debley, J. S., Redding, G. J., & Critchlow, C. W. (2004). Impact of adolescence and gender on asthma hospitalization: A population-based birth cohort study. Pediatric Pulmonology, 38(6), 443–450.
Kurpas, D., Rudkowski, Z., & Steciwko, A. (2005). The tobacco smoke as the main factor of in-door pollution in the aspect of the children health. Przeglad Lekarski, 62(10), 1173–1175.
Perez-Padilla, R., Rojas, R., Torres, V., Borja-Aburto, V., Olaiz, G., & The Empece Working G. (2006). Obesity among children residing in Mexico City and its impact on lung function: A comparison with Mexican-Americans. Archives of Medical Research, 37(1), 165–171.
Smith, O. O., & Helms, P. J. (2001). Genetic/environmental determinants of adult chronic obstructive pulmonary disease and possible links with childhood wheezing. Paediatric Respiratory Reviews, 2(2), 178–183.
Alper, Z., Sapan, N., Ercan, I., Canitez, Y., & Bilgel, N. (2006). Risk factors for wheezing in primary school children in Bursa, Turkey. American Journal of Rhinology, 20(1), 53–63.
Genuneit, J., Weinmayr, G., Radon, K., Dressel, H., Windstetter, D., Rzehak, P., et al. (2006). Smoking and the incidence of asthma during adolescence: Results of a large cohort study in Germany. Thorax, 61(7), 572–578.
Gilliland, F. D., Li, Y. F., & Peters, J. M. (2001). Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. American Journal of Respiratory and Critical Care Medicine, 163(2), 429–436.
Kelly, Y. J., Brabin, B. J., Milligan, P., Heaf, D. P., Reid, J., & Pearson, M. G. (1995). Maternal asthma, premature birth, and the risk of respiratory morbidity in schoolchildren in Merseyside. Thorax, 50(5), 525–530.
Acknowledgments
The assistance of Mr Gregory Harper, Mrs Farideh Yavandi and Mr Mostafa Delpisheh as well as the cooperation of parents and head teachers are gratefully acknowledged. This study was funded by a grant from the Sefton Health Authority.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Delpisheh, A., Kelly, Y., Rizwan, S. et al. Salivary Cotinine, Doctor-diagnosed Asthma and Respiratory Symptoms in Primary Schoolchildren. Matern Child Health J 12, 188–193 (2008). https://doi.org/10.1007/s10995-007-0229-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-007-0229-9