Abstract
Objective
Protein energy malnutrition (PEM) is a nutritional problem affecting many children world-wide. Its association with a wide spectrum of infections necessitates multiple drug therapies. A systematic review was performed to determine the effects of PEM on drug pharmacokinetics.
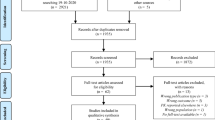
Methods
Literature searches in the MEDLINE and EMBASE databases (January 1960 to December 2009) were performed. Malnutrition, undernutrition, underweight, protein-energy malnutrition, protein-calorie malnutrition, marasmus, marasmic-kwashiorkor or kwashiorkor was the medical subject heading (MeSH) descriptor used. Inclusion criteria were abstracts that assessed or discussed absorption, distribution, metabolism, elimination, clearance, pharmacokinetics or pharmacodynamics of drugs, except micronutrients and appetite-stimulating drugs.
Results
Altogether, 41 publications were identified. A total of 34 drugs were studied. The absorption of 18 drugs was studied; the extent of absorption (AUC) was unaffected for 10 drugs. The plasma protein binding of 20 drugs was evaluated; it was significantly reduced for 12 drugs. The volume of distribution (Vd) of 13 drugs was evaluated; it was, however, unaffected for most of the drugs. The effect of PEM on total clearance and the half-life of drugs primarily metabolised by the liver was studied for 8 drugs. There was decreased total clearance and an associated increased half-life of 5 drugs. For 2 drugs (chloramphenicol and quinine), different degrees of PEM affected total clearance differently. The total clearance of six drugs primarily eliminated by the kidneys was studied; it was unaffected for four drugs, but significantly decreased for two drugs (cefoxitin and penicillin).
Conclusions
Considering the proportion of children affected with PEM world-wide, there have been relatively few pharmacokinetic studies of drugs frequently used for their treatment. More studies are therefore required to establish the appropriate dose and safety of these drugs for PEM children. The studies need to recognise that PEM is a disease spectrum and should further look at the differential effects of kwashiorkor and marasmus on drug pharmacokinetics in children.

Similar content being viewed by others
References
Collins S, Dent N, Binns P, Bahwere P, Sadler K, Hallam A (2006) Management of severe acute malnutrition. Lancet 368:1992–2000
Nnakwe N (1995) The effect and causes protein-energy malnutrition in Nigerian children. Nutr Res 15:785–794
World Health Organization (2005) Nutrition: challenges. Available at http://www.who.int/nutrition/challenges. Accessed October 2008
Fagule D (1990) Malnutrition: a reappraisal of the major predisposing factors. Niger J Paediatr 17:7–13
Schaible U, Kaufmann SHE (2007) Malnutrition and infection: complex mechanisms and global impacts. PLoS Med 4:e115
World Health Organization (2000) Management of the child with serious infection or severe malnutrition. Geneva: WHO/FCH/CAH/00.1. Available at http://www.helid.desastres.net/gsdl2/tmp/export/who/who89e.pdf. Accessed October 2008
Krishnaswamy K (1989) Drug metabolism and pharmacokinetics in malnourished children. Clin Pharmacokinet 17:68–88
Wellcome Trust Working Party (1970) Classification of infantile malnutrition. Lancet 2:302–303
Gomez F, Galvan RR, Frenk S, Munoz JC, Chavez R, Vazquez J (1956) Mortality in second and third degree malnutrition. J Trop Pediatr 2:77–83
Akbani Y, Bolme P, Lindblad BS, Rahimtoola RJ (1977) Control of streptomycin and isoniazid in malnourished children treated for tuberculosis. Acta Paediatr Scand 66:237–240
Erikksson M, Bolme P, Habte D, Paalzow L (1988) INH and streptomycin in Ethiopian children with tuberculosis and different nutritional status. Acta Paediatr Scand 77:890–894
Buchanan N, Hansen JDL, Van der Walt LA, Robinson R, Koornhof HJ (1976) Chloramphenicol metabolism in children with PCM. Am J Clin Nutr 29:327–330
Larea-Asseff I, Cravioto J, Santiago P, Perez-Ortiz B (1993) A new dosing regimen for metronidazole in malnourished children. Scand J Infect Dis 25:115–121
Seaton C, Ignas J, Muchohi S, Kokwaro G, Maitland K, Thomson AH (2007) Population pharmacokinetics of a single daily intramuscular dose of gentamicin in children with severe malnutrition. J Antimicrob Chemother 59:681–689
Treluyer JM, Sultan E, Alexandre JA, Roux A, Flouvat AB, Lagardere B (1991) Pharmacokinetics of aspirin in African children: influence of nutritional status. Arch Fr Pediatr 48:337–341
Graham SM, Bell DJ, Nyirongo S, Hartkoorn R, Ward SA, Molyneux EM (2006) Low levels of pyrazinamide and ethambutol in children with tuberculosis and impact of age, nutritional status, and human immunodeficiency virus infection. Antimicrob Agents Chemother 50:407–413
Samotra K, Gupte S, Raina RK (1985) Pharmacokinetics of gentamicin in protein-energy malnutrition. Eur J Clin Pharmacol 29:255–256
Larea-Asseff I, Cravioto J, Santiago P, Perez-Ortiz B (1992) Pharmacokinetics of metronidazole in severely malnourished and nutritionally rehabilitated children. Clin Pharmacol Ther 51:42–50
Bolme P, Eriksson M, Paalzow L, Stintzing G, Zerihun G, Woldemariam T (1995) Malnutrition and pharmacokinetics of penicillin in Ethiopian children. Pharmacol Toxicol 76:259–262
Bano G, Sharma DB, Raina RK (1985) Pharmacokinetics of phenytoin in protein energy malnutrition. Indian J Pharmacol 17:77–78
Treluyer JM, Roux A, Mugnier C, Flouvat B, Largadere B (1996) Metabolism of quinine in children with global malnutrition. Pediatr Res 40:558–563
Kumar L, Garg SK, Singh S, Lal R, Shukla VK (1989) Theophylline pharmacokinetics in well-nourished and malnourished asthmatic children. Int J Clin Pharmacol Ther Toxicol 27:588–592
Buchanan N, Eyberg C (1978) Intramuscular tobramycin administration in kwashiorkor. S Afr Med J 53:273–274
Bano G, Raina RK, Sharma DB (1986) Pharmacokinetics of carbamazepine in protein energy malnutrition. Pharmacology 32:232–236
Walker O, Dawodu AH, Salako LA, Alvan G, Johnson AOK (1987) Single disposition of chloroquine in kwashiorkor and normal children—evidence for decreased absorption in kwashiorkor. Br J Clin Pharmacol 23:467–472
Akinyinka OO, Sowunmi A, Honeywell R, Renwick AG (2000) The pharmacokinetics of caffeine in Nigerian children suffering from malaria and kwashiorkor. Eur J Clin Pharmacol 56:153–158
Mehta S, Kalsi HK, Jayaraman S, Mathur VS (1975) Chloramphenicol metabolism in children with protein-calorie malnutrition. Am J Clin Nutr 28:977–981
Mehta S, Nain CK, Yadav D, Sharma B, Mathur VS (1985) Disposition of acetaminophen in children with protein calorie malnutrition. Int J Clin Pharmacol Ther Toxicol 23:311–315
Syed GB, Sharma DB, Raina RK (1986) Pharmacokinetics of phenobarbitone in protein energy malnutrition. Dev Pharmacol Ther 9:317–322
Salako LA, Sowunmi A, Akinbami FO (1989) Pharmacokinetics of quinine in African children suffering from kwashiorkor. Br J Clin Pharmacol 28:197–201
Mehta S, Nain CK, Sharma B, Mathur VS (1980) Metabolism of sulfadiazine in children with protein calorie malnutrition. Pharmacology 21:369–374
Bravo IG, Bravo ME, Plate G, Merlez J, Arancibia A (1984) The pharmacokinetics of cotrimoxazole sulphonamide in malnourished (Marasmic) infants. Pediatr Pharmacol (New York) 4:167–176
Eriksson M, Paalzow L, Bolme P, Mariam TW (1983) Chloramphenicol pharmacokinetics in Ethiopian children of differing nutritional status. Eur J Clin Pharmacol 24:819–823
Buchanan N, Van der Walt LA (1997) Chloramphenicol binding to normal and kwashiorkor sera. Am J Clin Nutr 30:847–850
Buchanan N (1977) Drug-protein binding and protein energy malnutrition. S Afr Med J 52:733–737
Buchanan N, Van der Walt LA, Strickwold B (1976) Pharmacology of malnutrition. III. Binding of digoxin to normal and kwashiorkor serum. J Pharm Sci 65:914–916
Buchanan N, Van der Walt LA (1977) The binding of antituberculous drugs to normal and kwashiorkor serum. S Afr Med J 52:522–525
Eyberg C, Moodley GP, Buchanan N (1974) The pharmacology of malnutrition. I. Salicylate binding studies using normal/plasma kwashiorkor serum. S Afr Med J 48:2564–2577
Buchanan N, Van der Walt LA (1977) The binding of thiopentone to kwashiorkor serum. Br J Anaesth 49:247–250
Buchanan N, Van der Walt LA (1977) The binding of chloroquine to normal and kwashiorkor serum. Am J Trop Med Hyg 26:1025–1027
Buchanan N, Davis MD, Henderson DB, Mucklow JC, Rawlins MD (1980) Acetanilide pharmacokinetics in kwashiorkor. Br J Clin Pharmacol 9:525–526
Hendricks MK, Van der Bijl P, Parkin DP, Donald PR (1995) Pharmacokinetics of amikacin in children with kwashiorkor. Ann Trop Paediatr 15:295–298
Narang RK, Mehta S, Mathur VS (1977) Pharmacokinetic study of antipyrine in malnourished children. Am J Clin Nutr 30:1979–1982
Buchanan N, Eyberg C, Davis MD (1979) Antipyrine pharmacokinetics and D-glutaric excretion in kwashiorkor. Am J Clin Nutr 32:2439–2442
Homeida M, Karrar ZA, Roberts CJC (1979) Drug metabolism in malnourished children: a study with antipyrine. Arch Dis Child 54:299–302
Buchanan N, Eyberg C, Davis MD (1979) Isoniazid pharmacokinetics in kwashiorkor. S Afr Med J 56:299–300
Buchanan N, Robinson P, Koornhof HJ, Eyberg C (1979) Penicillin pharmacokinetics in kwashiorkor. Am J Clin Nutr 32:2233–2236
Bolme P, Eriksson M, Habte D, Paalzow L (1988) Pharmacokinetics of streptomycin in Ethiopian children with tuberculosis and different nutritional status. Eur J Clin Pharmacol 33:647–649
Eriksson M, Paalzow L, Bolme P, Mariam TW (1983) Pharmacokinetics of theophylline in Ethiopian children of differing nutritional status. Eur J Clin Pharmacol 24:89–92
Bravo ME, Arancibia A, Jarpa S, Carpentier PM, Jahn AN (1982) Pharmacokinetics of gentamicin in malnourished infants. Eur J Clin Pharmacol 21:499–504
Pussard E, Barennes H, Daouda H, Clavier F, Sani AM, Osse M, Granic G, Verdier F (1999) Quinine disposition in globally malnourished children with cerebral malaria. Clin Pharmacol Ther 65:500–510
Buchanan N, Davis MD, Eyberg C (1979) Gentamicin pharmacokinetics in kwashiorkor. Br J Clin Pharmacol 8:451–453
Buchanan N, Mithal Y, Witcomb M (1980) Cefoxitin: intravenous pharmacokinetics and intramuscular bioavailability in kwashiorkor. Br J Clin Pharmacol 9:623–627
Mehta S, Nain CK, Sharma B, Mathur VS (1982) Disposition of four drugs in malnourished children. Drug Nutr Interact 1:205–211
Seifart HI, Donald PR, De Villiers JN, Parkin DP, Jaarsveld PP (1995) Isoniazid elimination kinetics in children with protein-energy malnutrition treated for tuberculous meningitis with a four-component antimicrobial regimen. Ann Trop Paediatr 15:249–254
Cohen-Kohler JC (2007) The morally uncomfortable global drug gap. Clin Pharmacol Ther 82:610–614
De Onis M, Frongillo EA, Blössner M (2000) Is malnutrition declining? An analysis of changes in levels of child malnutrition since 1980. Bull World Health Organ 78:1222–1233
Khor GL (2003) Update on the prevalence of malnutrition among children in Asia. Nepal Med Coll J 5:113–122
Trouiller P, Olliaro P, Torreele E, Orbinski J et al (2002) Drug development for neglected diseases: a deficient market and public-health policy failure. Lancet 359:2188–2194
Clark J (2003) Euro MPs vote on research fund for neglected diseases. Br Med J 326:680
Faull R, Lee L (2007) Prescribing in renal disease. Aust Prescr 30:17–20
Mutabingwa TK (2005) Artemisinin-based combination therapies (ACTs): best hope for malaria treatment but inaccessible to the needy! Acta Trop 95:305–315
World Health Organization (2006) Guidelines for the treatment of malaria. WHO. Available at: http://apps.who.int/malaria/docs/TreatmentGuidelines2006.pdf. Accessed November 2009
Projean D, Baune B, Farinotti R, Flinois J, Beaune P, Taburet A, Ducharme J (2003) In-vitro metabolism of chloroquine: identification of CYP2C8, CYP3A4, and CYP2D6 as the main isoforms catalyzing N-desethylchloroquine formation. Drug Metab Disp 31:748–754
German PI, Aweeka FT (2008) Clinical pharmacology of artemisinin-based combination therapies. Clin Pharmacokinet 47:91–102
Rylance G (1981) Drugs in children. BMJ 282:50–51
Churchwell MD, Pasko DA, Smoyer WE, Mueller BA (2009) Enhanced clearance of highly protein-bound drugs by albumin-supplemented dialysate during modelled continuous hemodialysis. Nephrol Dial Transplant 24:231–238
Thomson AH (2006) Population pharmacokinetics and pharmacodynamics. In: Jacqz-Aigrain E, Choonara I (eds) Paediatric clinical pharmacology, 1st edn. Fontis Media S.A./Taylor & Francis Group, London/New York, pp 147–159
Parker AC, Pritchard P, Preston T, Smyth RL et al (1997) Enhanced drug metabolism in young children with cystic fibrosis. Arch Dis Child 77:239–241
Pons G, Blais JC, Rey E, Plissonnier M et al (1988) Maturation of caffeine N-demethylation in infancy: a study using the 13CO2 breath test. Pediatr Res 11:258–264
Choonara I (2009) Children’s medicines—a global problem. Arch Dis Child 94:467
Acknowledgements
KAO is a postgraduate research student being jointly sponsored by the Lagos State Government and the Lagos State University, Ojo, Lagos, Nigeria. The authors acknowledge these sponsoring bodies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oshikoya, K.A., Sammons, H.M. & Choonara, I. A systematic review of pharmacokinetics studies in children with protein-energy malnutrition. Eur J Clin Pharmacol 66, 1025–1035 (2010). https://doi.org/10.1007/s00228-010-0851-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0851-0