Abstract
Abstract
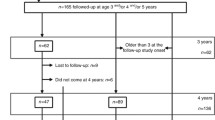
Little is known about serum creatinine concentration, urinary creatinine excretion and creatinine clearance in preterm infants. The aim of the present study was to establish age related reference values for the first weeks of life in preterm infants with a birth weight<1500 g. In addition, the possible influence of therapy with dexamethasone, spironolactone and catecholamines was investigated. In 34 patients, serum creatinine, urinary creatinine excretion and creatinine clearance were measured at weeks 1, 2, 3–4, 5–6 and 7–9 of life. Median birth weight was 1225 g (range 730–1495), mean gestational age 29 (range 26–34) weeks. Concentration of creatinine in serum and urine, urinary creatinine excretion per kilogram body weight and creatinine clearance showed a significant correlation with postnatal age. Thus age related reference values as proposed given in the present study are desirable. Median serum creatinine concentration decreased continuously within the first weeks of life: 97 (10–90th percentile: 69–141) in the 1st week, 70 (45–99) in the 2nd week, 57 (39–71) at week 3–4, 51 (42–62) at week 5–6 and 44 (39–48) μmol/l at week 7–9. Median creatinine output in μmol/kg body weight was 100 (10–90th percentile: 62–160) in the 1st week, 92 (65–120) in the 2nd week, 79 (52–122) at week 3–4, 89 (68–106) at week 5–6 and 86 (54–109) μmol/kg/d at week 7–9. Creatinine clearance increased significantly within the first weeks of life. Values were 12.5 (10–90 the percentile: 7–22) in the 1st week, 16 (10–28) in the 2nd week, 20 (11–34) at weeks 3–4, 23 (15–36) at weeks 5–6 and 29 (17–36) ml/min per 1.73 m2 at weeks 7–9. Therapy with dexamethasone, spironolactone or catecholamines showed no influence on creatinine excretion. Creatinine clearance did not only depend on postnatal age but also on gestational age and on the necessity of mechanical ventilation. These findings indicate a reduced glomerular filtration rate in very immature and severely ill preterm infants.
Conclusion
It might be necessary to lower dosage of renal excreted drugs in very immature and mechanically ventilated infants according to the creatinine clearance.
Similar content being viewed by others
References
Al-Dahhan J, Haycock GB, Chantler C, Stimmler L (1983) Sodium homeostasis in term and preterm neonates. I. Renal aspects. Arch Dis Child 58:335–342
Al-Dahhan J, Stimmler L, Chantler C, Haycock GB (1988) Urinary creatinine excretion in the newborn, Arch Dis Child 63:398–402
Aperia A, Broberger O, Elinder G, Herin P, Zetterström R (1981) Postnatal development of renal function in pre-term and full-term infants. Acta Pacdiatr Scand 70:183–187
Aperia A, Broberger O, Herin P, Thodenius K, Zetterström R (1983) Postnatal control of water and electrolyte homeostasis in pre-term and full-term infants. Acta Paediatr Scand [Suppl] 305:61–65
Brion LP, Fleischman AR, McCarton C, Schwartz GJ (1986) A simple estimate of glomerular filtration rate in low birth weight infants during the first year of life: Noninvasive assesment of body composition and growth. J Pediatr 109:698–707
Burghard R, Leititis JU, Brandis M (1987) Nierenfunktionsstörungen und akutes Nierenversagen bei Neugeborenen. Monatsschr Kinderheilkd 135:10–21
Feldman H, Guignard JP (1982) Plasma creatinine in the first month of life. Arch Dis Child 57:123–126
Gordjani N, Burghard R, Leititis JU, Brandis M (1988) Serum creatinine and creatinine clearance in healthy neonates and prematures during the first 10 days of life. Eur J Pediatr 148:143–145
Guignard JP, Torrado A, Da Cunha O, Gautier E (1975) Glomerular filtration rate in the first three weeks of life. J Pediatr 87:268–272
Leititis JU, Burghard R, Gordjani N, Kaethner T, Brandis M (1987) Entwicklungsphysiologische Aspekte der Volumen- und Natriumregulation bei Frühgeborenen und reifen Neugeborenen. Monatsschr Kinderheilkd 135:3–9
Ross B, Cowett RM, Oh W (1977) Renal functions of low birth weight infants during the first two months of life. Pediatr Res 11:1162–1164
Sertel H, Scopes J (1973) Rates of creatinine clearance in babies less than one week of age. Arch Dis Child 48: 717–720
Siegel SR, Oh W (1976) Renal function as a marker of human fetal maturation. Acta Paediatr Scand 65:481–485
Stonestreet BS, Oh W (1978) Plasma creatinine levels in low-birth-weight infants during the first three months of life. Pediatrics 61:788–789
Sutphen JL (1982) Anthropometric determinants of creatinine excretion in preterm infants. Pediatrics 69:719–723
Zanardo V, Da Riol R, Marchesini L, Largajolli G, Zachello G (1991) Renal function in preterm twins with birth weight discordance. Child Nephrol Urol 11:87–90
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sonntag, J., Prankel, B. & Waltz, S. Serum creatinine concentration, urinary creatinine excretion and creatinine clearance during the first 9 weeks in preterm infants with a birth weight below 1500 g. Eur J Pediatr 155, 815–819 (1996). https://doi.org/10.1007/BF02002914
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02002914