Abstract
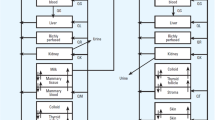
There are many benefits of breast-feeding both for the infant and for the mother. Nursing mothers who are also taking medications or exposed to environmental hazards may be confronted with a difficult choice to discontinue nursing or maternal medication or risk potential harm to the infant. Frequently, these decisions are made without sufficient information or understanding of the factors influencing exposure. The current review explores two indices of exposure, together with their pharmacokinetic determinants. Both of the indices include the milk to serum (M/S) concentration ratio for a given drug and the volume of milk consumed. The first exposure term, EI(Dose), expresses neonatal dose as a percentage of maternal dose and is inversely related to the maternal systemic clearance. By contrast, the second exposure term, EI(Conc), expresses infant concentration as a percentage of maternal concentration and is inversely related to the infant systemic clearance. Issues related to intersubject variation in M/S (e.g., colostrum vs. mature milk, fore vs. hind milk) and infant clearance (e.g., ontogeny of elimination pathways, pharmacogenetics) and their role in modulating exposure are also discussed.
Similar content being viewed by others
References
A. L. Wright. The rise of breastfeeding in the United States. Pediatr. Clin. North Am. 48:1-12 (2001).
A. Wrightand and R. Schanler. The resurgence of breastfeeding at the end of the second millennium. J. Nutr. 131:421S-425S (2001).
H. Vorherr. The Breast, Academic Press, New York, 1974.
J. Wilson. Drugs in Breast Milk, ADIS Press, Auckland, 1981.
E. L. Mortensen, K. F. Michaelsen, S. A. Sanders, and J. M. Reinisch. The association between duration of breastfeeding and adult intelligence. JAMA 287:2365-2371 (2002).
Collaborative Group on Hormonal Factors in Breast Cancer Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet 360:187-195 (2002).
S. L. Hatcher. The psychological experience of nursing mothers upon learning of a toxic substance in their breast milk. Psychiatry 45:172-181 (1982).
P. Bennet. Drugs and Human Lactation, Elsevier, Amsterdam, 1988.
P. O. Anderson. Drug use during breast-feeding. Clin. Pharm. 10:594-624 (1991).
S. Ito. Drug therapy for breast-feeding women. N. Engl. J. Med. 343:118-126 (2000).
C. M. BerlinJr. Drugs and chemicals: exposure of the nursing mother. Pediatr. Clin. North Am. 36:1089-1097 (1989).
S. A. Banta-Wright. Minimizing infant exposure to and risks from medications while breastfeeding. J. Perinat. Neonatal. Nurs. 11:71-84; quiz 85–86 (1997).
H. C. Atkinson, E. J. Begg, and B. A. Darlow. Drugs in human milk. Clinical pharmacokinetic considerations. Clin. Pharmacokinet. 14:217-240 (1988).
J. T. Wilson, R. D. Brown, D. R. Cherek, J. W. Dailey, B. Hilman, P. C. Jobe, B. R. Manno, J. E. Manno, H. M. Redetzki, and J. J. Stewart. Drug excretion in human breast milk: principles, pharmacokinetics and projected consequences. Clin. Pharmacokinet. 5:1-66 (1980).
J. T. Wilson. Determinants and consequences of drug excretion in breast milk. Drug Metab. Rev. 14:619-652 (1983).
J. T. Wilson, R. D. Brown, J. L. Hinson, and J. W. Dailey. Pharmacokinetic pitfalls in the estimation of the breast milk/plasma ratio for drugs. Annu. Rev. Pharmacol. Toxicol. 25:667-689 (1985).
C. M. Berlin. The excretion of drugs in human milk. Prog. Clin. Biol. Res. 36:115-127 (1980).
C. M. BerlinJr. Pharmacologic considerations of drug use in thelactating mother. Obstet. Gynecol. 58:17S-23S (1981).
J. C. Fleishaker, N. Desai, and P. J. McNamara. Factors affecting the milk-to-plasma drug concentration ratio in lactating women: physical interactions with protein and fat. J. Pharm. Sci. 76:189-193 (1987).
H. C. Atkinson and E. J. Begg. Prediction of drug distribution into human milk from physicochemical characteristics. Clin. Pharmacokinet. 18:151-167 (1990).
S. Ito and A. Lee. Drug excretion into breast milk—overview. Adv. Drug Deliv. Rev. 55:617-627 (2003).
J. C. Fleishaker. Models and methods for predicting drug transfer into human milk. Adv. Drug Deliv. Rev. 55:643-652 (2003).
K. Yoshida, B. Smith, M. Craggs, and R. C. Kumar. Fluoxetine in breast-milk and developmental outcome of breast-fed infants. Br. J. Psychiatry 172:175-178 (1998).
V. Hendrick, A. Fukuchi, L. Altshuler, M. Widawski, A. Wertheimer, and M. V. Brunhuber. Use of sertraline, paroxetine and fluvoxamine by nursing women. Br. J. Psychiatry 179:163-166 (2001).
V. Hendrick, Z. N. Stowe, L. L. Altshuler, J. Mintz, S. Hwang, A. Hostetter, R. Suri, K. Leight, and A. Fukuchi. Fluoxetine and norfluoxetine concentrations in nursing infants and breast milk. Biol. Psychiatry 50:775-782 (2001).
N. Epperson, K. A. Czarkowski, D. Ward-O'Brien, E. Weiss, R. Gueorguieva, P. Jatlow, and G. M. Anderson. Maternal sertraline treatment and serotonin transport in breast-feeding mother-infant pairs. Am. J. Psychiatry 158:1631-1637 (2001).
C. M. Berlin. Sensitivity of the young infant to drug exposure through human milk. Adv. Drug Deliv. Rev. 55:687-693 (2003).
S. Ito and G. Koren. A novel index for expressing exposure of the infant to drugs in breast milk. Br. J. Clin. Pharmacol. 38:99-102 (1994).
M. C. Neville and C. T. Walsh. Effects of xenobiotics on milk secretion and composition. Am. J. Clin. Nutr. 61:687S-694S (1995).
J. L. Dorne, K. Walton, and A. G. Renwick. Uncertainty factors for chemical risk assessment. Human variability in the pharmacokinetics of CYP1A2 probe substrates. Food Chem. Toxicol. 39:681-696 (2001).
J. L. Brazier, J. Ritter, M. Berland, D. Khenfer, and G. Faucon. Pharmacokinetics of caffeine during and after pregnancy. Dev. Pharmacol. Ther. 6:315-322 (1983).
J. V. Aranda, J. M. Collinge, R. Zinman, and G. Watters. Maturation of caffeine elimination in infancy. Arch. Dis. Child. 54:946-949 (1979).
C. Y. Oo, D. E. Burgio, R. C. Kuhn, N. Desai, and P. J. McNamara. Pharmacokinetics of caffeine and its demethylated metabolites in lactation: predictions of milk to serum concentration ratios. Pharm. Res. 12:313-316 (1995).
M. C. Neville and J. Morton. Physiology and endocrine changes underlying human lactogenesis II. J. Nutr. 131:3005S-3008S (2001).
G. M. Chan. Lactation: the Breast-Feeding Manual for Health Professionals, Precept, Chicago, 1997.
L. Borgatta, R. W. Jenny, L. Gruss, C. Ong, and D. Barad. Clinical significance of methohexital, meperidine, and diazepam in breast milk. J. Clin. Pharmacol. 37:186-192 (1997).
V. L. Feilberg, D. Rosenborg, C. Broen Christensen, and J. V. Mogensen. Excretion of morphine in human breast milk. Acta Anaesthesiol. Scand. 33:426-428 (1989).
N. E. Baka, F. Bayoumeu, M. J. Boutroy, and M. C. Laxenaire. Colostrum morphine concentrations during postcesarean intravenous patient-controlled analgesia. Anesth. Analg. 94:184-187 (2002).
Z. Esener, B. Sarihasan, H. Guven, and E. Ustun. Thiopentone and etomidate concentrations in maternal and umbilical plasma, and in colostrum. Br. J. Anaesth. 69:586-588 (1992).
L. W. Andersen, T. Qvist, J. Hertz, and F. Mogensen. Concentrations of thiopentone in mature breast milk and colostrum following an induction dose. Acta Anaesthesiol. Scand. 31:30-32 (1987).
K. Yoshida, B. Smith, M. Craggs, and R. C. Kumar. Investigation of pharmacokinetics and of possible adverse effects in infants exposed to tricyclic antidepressants in breast-milk. J. Affect. Disord. 43:225-237 (1997).
Z. N. Stowe, L. S. Cohen, A. Hostetter, J. C. Ritchie, M. J. Owens, and C. B. Nemeroff. Paroxetine in human breast milk and nursing infants. Am. J. Psychiatry 157:185-189 (2000).
Z. N. Stowe, M. J. Owens, J. C. Landry, C. D. Kilts, T. Ely, A. Llewellyn, and C. B. Nemeroff. Sertraline and desmethylsertraline in human breast milk and nursing infants. Am. J. Psychiatry 154:1255-1260 (1997).
M. F. Goldfarb and M. S. Savadove. Creamatocrit and pH measurements of human milk. J. Pediatr. Gastroenterol. Nutr. 12:142-143 (1991).
J. H. Kristensen, K. F. Ilett, L. P. Hackett, P. Yapp, M. Paech, and E. J. Begg. Distribution and excretion of fluoxetine and norfluoxetine in human milk. Br. J. Clin. Pharmacol. 48:521-527 (1999).
J. H. Kristensen, K. F. Ilett, L. J. Dusci, L. P. Hackett, P. Yapp, R. E. Wojnar-Horton, M. J. Roberts, and M. Paech. Distribution and excretion of sertraline and N-desmethylsertraline in human milk. Br. J. Clin. Pharmacol. 45:453-457 (1998).
J. Rampono, J. H. Kristensen, L. P. Hackett, M. Paech, R. Kohan, and K. F. Ilett. Citalopram and demethylcitalopram in human milk; distribution, excretion and effects in breast fed infants. Br. J. Clin. Pharmacol. 50:263-268 (2000).
S. Kaneko, T. Sato, and K. Suzuki. The levels of anticonvulsants in breast milk. Br. J. Clin. Pharmacol. 7:624-627 (1979).
W. Kuhnz, S. Koch, H. Helge, and H. Nau. Primidone and phenobarbital during lactation period in epileptic women: total and free drug serum levels in the nursed infants and their effects on neonatal behavior. Dev. Pharmacol. Ther. 11:147-154 (1988).
W. Froescher, M. Eichelbaum, M. Niesen, K. Dietrich, and P. Rausch. Carbamazepine levels in breast milk. Ther. Drug Monit. 6:266-271 (1984).
J. Alcorn, X. Lu, J. A. Moscow, and P. J. McNamara. Transporter gene expression in lactating and nonlactating human mammary epithelial cells using real-time reverse transcription-polymerase chain reaction. J. Pharmacol. Exp. Ther. 303:487-496 (2002).
S. Ito and J. Alcorn. Xenobiotic transporter expression and function in the human mammary gland. Adv. Drug Deliv. Rev. 55:653-665 (2003).
C. Y. Oo, R. J. Kuhn, N. Desai, and P. J. McNamara. Active transport of cimetidine into human milk. Clin. Pharmacol. Ther. 58:548-555 (1995).
P. M. Gerk, R. J. Kuhn, N. S. Desai, and P. J. McNamara. Active transport of nitrofurantoin into human milk. Pharmacotherapy 21:669-675 (2001).
J. Alcorn and P. J. McNamara. the ontogeny of hepatic and renal systemic clearance pathways in infants: a review (part I). Clin. Pharmacokinet. 41:959-998 (2002).
J. Alcorn and P. J. McNamara. The ontogeny of hepatic and renal systemic clearance pathways in infants: model predictions (part II). Clin. Pharmacokinet. 41:1077-1094 (2002).
J. Alcorn and P. J. McNamara. Pharmacokinetics in the newborn. Adv. Drug Deliv. Rev. 55:667-686 (2003).
T. Cresteil. Onset of xenobiotic metabolism in children: toxicological implications. Food Addit. Contam. 15:45-51 (1998).
S. Caccia. Metabolism of the newer antidepressants. An overview of the pharmacological and pharmacokinetic implications. Clin. Pharmacokinet. 34:281-302 (1998).
C. Hiemke and S. Hartter. Pharmacokinetics of selective serotonin reuptake inhibitors. Pharmacol. Ther. 85:11-28 (2000).
H. L. McLeod and W. E. Evans. Pharmacogenomics: unlocking the human genome for better drug therapy. Annu. Rev. Pharmacol. Toxicol. 41:101-121 (2001).
O. Spigset and S. Hagg. Excretion of psychotropic drugs into breast milk; pharmacokinetic overview and therapeutic implications. CNS Drugs 9:111-134 (1998).
L. Bertilsson, M. L. Dahl, P. Dalen, and A. Al-Shurbaji. Molecular genetics of CYP2D6: clinical relevance with focus on psychotropic drugs. Br. J. Clin. Pharmacol. 53:111-122 (2002).
J. H. Kristensen, L. P. Hackett, R. Kohan, M. Paech, and K. F. Ilett. The amount of fluvoxamine in milk is unlikely to be a cause of adverse effects in breastfed infants. J. Hum. Lact. 18:139-143 (2002).
E. J. Begg, S. B. Duffull, D. A. Saunders, R. C. Buttimore, K. F. Ilett, L. P. Hackett, P. Yapp, and D. A. Wilson. Paroxetine in human milk. Br. J. Clin. Pharmacol. 48:142-147 (1999).
K. F. Ilett, L. P. Hackett, L. J. Dusci, M. J. Roberts, J. H. Kristensen, M. Paech, A. Groves, and P. Yapp. Distribution and excretion of venlafaxine and O-desmethylvenlafaxine in human milk. Br. J. Clin. Pharmacol. 45:459-462 (1998).
N. Poolsup, A. Li Wan Po, and T. L. Knight. Pharmacogenetics and psychopharmacotherapy. J. Clin. Pharm. Ther. 25:197-220 (2000).
C. R. Howard and R. A. Lawrence. Drugs and breastfeeding. Clin. Perinatol. 26:447-478 (1999).
M. J. Boutroy, G. Bianchetti, C. Dubruc, P. Vert, and P. L. Morselli. To nurse when receiving acebutolol: is it dangerous for the neonate? Eur. J. Clin. Pharmacol. 30:737-739 (1986).
G. Bianchetti, C. Dubroc, P. Vert, M. Boutroy, and P. Morselli. Placental transfer and pharmacokinetics of acebutolol in newborn infants. Clin. Pharmacol. Ther. 29:233-234 (1981).
B. N. Singh, W. R. Thoden, and J. Wahl. Acebutolol: a review of its pharmacology, pharmacokinetics, clinical uses, and adverse effects. Pharmacotherapy 6:45-63 (1986).
B. J. Anderson, N. H. Holford, G. A. Woollard, and P. L. Chan. Paracetamol plasma and cerebrospinal fluid pharmacokinetics in children. Br. J. Clin. Pharmacol. 46:237-243 (1998).
W. Kuhnz, E. Jager-Roman, D. Rating, A. Deichl, J. Kunze, H. Helge, and H. Nau. Carbamazepine and carbamazepine-10,11-epoxide during pregnancy and postnatal period in epileptic mother and their nursed infants: pharmacokinetics and clinical effects. Pediatr Pharmacol 3:199-208 (1983).
S. Pynnonen, J. Kanto, M. Sillanpaa, and R. Erkkola. Carbamazepine: placental transport, tissue concentrations in foetus and newborn, and level in milk. Acta Pharmacol. Toxicol. (Copenh.) 41:244-253 (1977).
L. Bertilsson and T. Tomson. Clinical pharmacokinetics and pharmacological effects of carbamazepine and carbamazepine-10,11-epoxide. An update. Clin. Pharmacokinet. 11:177-198 (1986).
E. Rey, P. d'Athis, D. de Lauture, O. Dulac, J. Aicardi, and G. Olive. Pharmacokinetics of carbamazepine in the neonate and in the child. Int. J. Clin. Pharmacol. Biopharm. 17:90-96 (1979).
J. Knowles. Drugs in milk. Pediatr. Currents 21:28-32 (1972).
P. Periti, T. Mazzei, E. Mini, and A. Novelli. Clinical pharmacokinetic properties of the macrolide antibiotics. Effects of age and various pathophysiological states (part II). Clin. Pharmacokinet. 16:261-282 (1989).
K. B. Waites, P. J. Sims, D. T. Crouse, M. H. Geerts, R. E. Shoup, W. B. Hamrick, L. B. Duffy, and G. H. Cassell. Serum concentrations of erythromycin after intravenous infusion in preterm neonates treated for ureaplasma urealyticum infection. Pediatr. Infect. Dis. J. 13:287-293 (1994).
X. Wagner, J. Jouglard, M. Moulin, A. M. Miller, J. Petitjean, and A. Pisapia. Coadministration of flecainide acetate and sotalol during pregnancy: lack of teratogenic effects, passage across the placenta, and excretion in human breast milk. Am. Heart J. 119:700-702 (1990).
R. L. McQuinn, A. Pisani, S. Wafa, S. F. Chang, A. M. Miller, J. M. Frappell, G. V. Chamberlain, and A. J. Camm. Flecainide excretion in human breast milk. Clin. Pharmacol. Ther. 48:262-267 (1990).
C. Funck-Brentano, L. Becquemont, H. K. Kroemer, K. Buhl, N. G. Knebel, M. Eichelbaum, and P. Jaillon. Variable disposition kinetics and electrocardiographic effects of flecainide during repeated dosing in humans: contribution of genetic factors, dose-dependent clearance, and interaction with amiodarone. Clin. Pharmacol. Ther. 55:256-269 (1994).
J. A. Till, E. A. Shinebourne, E. Rowland, D. E. Ward, R. Bhamra, P. Haga, A. Johnston, and D. W. Holt. Paediatric use of flecainide in supraventricular tachycardia: clinical efficacy and pharmacokinetics. Br. Heart J. 62:133-139 (1989).
T. H. Lebedevs, R. E. Wojnar-Horton, P. Yapp, M. J. Roberts, L. J. Dusci, L. P. Hackett, and K. F. Ilett. Excretion of indomethacin in breast milk. Br. J. Clin. Pharmacol. 32:751-754 (1991).
O. Eeg-Olofsson, I. Malmros, C. E. Elwin, and B. Steen. Convulsions in a breast-fed infant after maternal indomethacin. Lancet 2:215(1978).
R. Oberbauer, P. Krivanek, and K. Turnheim. Pharmacokinetics of indomethacin in the elderly. Clin. Pharmacokinet. 24:428-434 (1993).
M. Weninger, A. Pollak, U. Salzer-Muhar, K. A. Vergesslich, and H. R. Salzer. Pharmacokinetics of intra-arterial indomethacin treatment for patent ductus arteriosus. Eur. J. Pediatr. 149:138-140 (1989).
G. Briggs, R. Freeman, and S. Yaffe. Drugs in Pregnancy and Lactation, Williams & Wilkins, Baltimore, 1998.
J. Heykants, M. Michiels, W. Meuldermans, J. Monbaliu, K. Lavrijsen, A. Van Peer, J. Levran, R. Woestenbourghs, and G. Cauwenbergh. The pharmacokinetics or itraconazole in animals and man. An overview. In R. Fromtling (ed.), Recent Trends in the Discovery, Development and Evaluation of Antifungal Agents, Prous Science Publisher, Barcelona, 1987.
L. de Repentigny, J. Ratelle, J. M. Leclerc, G. Cornu, E. M. Sokal, P. Jacqmin, and K. De Beule. Repeated-dose pharmacokinetics of an oral solution of itraconazole in infants and children. Antimicrob. Agents Chemother. 42:404-408 (1998).
A. G. Whitelaw, A. J. Cummings, and I. R. McFadyen. Effect of maternal lorazepam on the neonate. Br. Med. J. (Clin. Res. Ed.) 282:1106-8 (1981).
R. J. Summerfield and M. S. Nielsen. Excretion of lorazepam into breast milk. Br. J. Anaesth. 57:1042-1043 (1985).
D. J. Greenblatt. Clinical pharmacokinetics of oxazepam and lorazepam. Clin. Pharmacokinet. 6:89-105 (1981).
W. R. Crom, M. V. Relling, M. L. Christensen, G. K. Rivera, and W. E. Evans. Age-related differences in hepatic drug clearance in children: studies with lorazepam and antipyrine. Clin. Pharmacol. Ther. 50:132-140 (1991).
C. A. McDermott, A. L. Kowalczyk, E. R. Schnitzler, H. H. Mangurten, K. A. Rodvold, and S. Metrick. Pharmacokinetics of lorazepamin critically ill neonates with seizures. J. Pediatr. 120:479-483 (1992).
A. Kauppila, P. Arvela, M. Koivisto, S. Kivinen, O. Ylikorkala, and O. Pelkonen. Metoclopramide and breast feeding: transfer into milk and the newborn. Eur. J. Clin. Pharmacol. 25:819-823 (1983).
K. Lauritsen, L. S. Laursen, and J. Rask-Madsen. Clinical pharmacokinetics of drugs used in the treatment of gastrointestinal diseases (Part II). Clin. Pharmacokinet. 19:94-125 (1990).
G. L. Kearns, J. N. van den Anker, M. D. Reed, and J. L. Blumer. Pharmacokinetics of metoclopramide in neonates. J. Clin. Pharmacol. 38:122-128 (1998).
G. L. Kearns, H. L. Butler, J. K. Lane, S. H. Carchman, and G. J. Wright. Metoclopramide pharmacokinetics and pharmacodynamics in infants with gastroesophageal reflux. J. Pediatr. Gastroenterol. Nutr. 7:823-829 (1988).
I. Matheson, P. K. Lunde, and J. E. Bredesen. Midazolam and nitrazepam in the maternity ward: milk concentrations and clinical effects. Br. J. Clin. Pharmacol. 30:787-793 (1990).
P. D. Garzone and P. D. Kroboth. Pharmacokinetics of the newer benzodiazepines. Clin. Pharmacokinet. 16:337-364 (1989).
T. C. Lee, B. G. Charles, G. J. Harte, P. H. Gray, P. A. Steer, and V. J. Flenady. Population pharmacokinetic modeling in very premature infants receiving midazolam during mechanical ventilation: midazolam neonatal pharmacokinetics. Anesthesiology 90:451-457 (1999).
P. Burtin, E. Jacqz-Aigrain, P. Girard, R. Lenclen, J. F. Magny, P. Betremieux, C. Tehiry, L. Desplanques, and P. Mussat. Population pharmacokinetics of midazolam neonates. Clin. Pharmacol. Ther. 56:615-625 (1994).
J. K. Marshall, A. B. Thompson, and D. Armstrong. Omeprazole for refractory gastroesophageal reflux disease during pregnancy and lactation. Can. J. Gastroenterol. 12:225-227 (1998).
M. Chang, G. Tybring, M. L. Dahl, E. Gotharson, M. Sagar, R. Seensalu, and L. Bertilsson. Interphenotype differences in disposition and effect on gastrin levels of omeprazole—suitability of omeprazole as a probe for CYP2C19. Br. J. Clin. Pharmacol. 39:511-518 (1995).
E. Jacqz-Aigrain, M. Bellaich, C. Faure, J. Andre, P. Rohrlich, V. Baudouin, and J. Navarro. Pharmacokinetics of intravenous omeprazole in children. Eur. J. Clin. Pharmacol. 47:181-185 (1994).
A. M. Yurchak and W. J. Jusko. Theophylline secretion into breast milk. Pediatrics 57:518-520 (1976).
G. P. Stec, P. Greenberger, T. I. Ruo, T. Henthorn, Y. Morita, A. J. AtkinsonJr., and R. Patterson. Kinetics of theophylline transfer to breast milk. Clin. Pharmacol. Ther. 28:404-408 (1980).
A. M. Taburet and B. Schmit. Pharmacokinetic optimisation of asthma treatment. Clin. Pharmacokinet. 26:396-418 (1994).
J. V. Aranda, D. S. Sitar, W. D. Parsons, P. M. Loughnan, and A. H. Neims. Pharmacokinetic aspects of theophylline in premature newborns. N. Engl. J. Med. 295:413-416 (1976).
J. T. Gilman, P. Gal, R. S. Levine, C. B. Hersh, and N. V. Erkan. Factors influencing theophylline disposition in 179 newborns. Ther. Drug Monit. 8:4-10 (1986).
H. W. Ahn, W. G. Shin, K. J. Park, O. K. Suh, and J. H. Choi. Pharmacokinetics of theophylline and caffeine after intravenous administration of aminophylline to premature neonates in Korea. Res. Commun. Mol. Pathol. Pharmacol. 105:105-113 (1999).
E. S. Moore, R. G. Faix, R. C. Banagale, and T. H. Grasela. The population pharmacokinetics of theophylline in neonates and young infants. J. Pharmacokinet. Biopharm. 17:47-66 (1989).
D. M. Hilligoss, W. J. Jusko, J. R. Koup, and G. Giacoia. Factors affecting theophylline pharmacokinetics in premature infants with apnea. Dev. Pharmacol. Ther. 1:6-15 (1980).
H. Nau, D. Rating, S. Koch, I. Hauser, and H. Helge. Valproic acid and its metabolites: placental transfer, neonatal pharmacokinetics, transfer via mother's milk and clinical status in neonates of epileptic mothers. J. Pharmacol. Exp. Ther. 219:768-777 (1981).
N. Tsuru, T. Maeda, and M. Tsuruoka. Three cases of delivery under sodium valproate—placental transfer, milk transfer and probable teratogenicity of sodium valproate. Jpn. J. Psychiatry Neurol. 42:89-96 (1988).
A. Philbert, B. Pedersen, and M. Dam. Concentration of valproate during pregnancy, in the newborn and in breast milk. Acta Neurol. Scand. 72:460-463 (1985).
G. Zaccara, A. Messori, and F. Moroni. Clinical pharmacokinetics of valproic acid—1988. Clin. Pharmacokinet. 15:367-389 (1988).
D. Battino, M. Estienne, and G. Avanzini. Clinical pharmacokinetics of antiepileptic drugs in paediatric patients. Part I: phenobarbital, primidone, valproic acid, ethosuximide and mesuximide. Clin. Pharmacokinet. 29:257-286 (1995).
L. Herngren, B. Lundberg, and A. Nergardh. Pharmacokinetics of total and free valproic acid during monotherapy in infants. J. Neurol. 238:315-319 (1991).
G. D. Morse, M. J. Shelton, and A. M. O'Donnell. Comparative pharmacokinetics of antiviral nucleoside analogues. Clin. Pharmacokinet. 24:101-123 (1993).
M. Mirochnick, E. Capparelli, and J. Connor. Pharmacokinetics of zidovudine in infants: a population analysis across studies. Clin. Pharmacol. Ther. 66:16-24 (1999).
M. Mirochnick, E. Capparelli, W. Dankner, R. S. Sperling, R. van Dyke, and S. A. Spector. Zidovudine pharmacokinetics in premature infants exposed to human immunodeficiency virus. Antimicrob. Agents Chemother. 42:808-812 (1998).
F. D. Boucher, J. F. Modlin, S. Weller, A. Ruff, M. Mirochnick, S. Pelton, C. Wilfert, R. McKinneyJr., M. J. Crain, M. M. Elkins, et al. Phase I evaluation of zidovudine administered to infants exposed at birth to the human immunodeficiency virus. J. Pediatr. 122:137-144 (1993).
J. M. Hopkinson, R. J. Schanler, J. K. Fraley, and C. Garza. Milk production by mothers of premature infants: influence of cigarette smoking. Pediatrics 90:934-938 (1992).
K. E. Thummel and D. Shen. Appendix II, design and optimization of dosage regimens; pharmacokinetic data. In L. Goodman, L. Limbird, P. Milinoff, A. Gilman, and J. Hardman (eds), The Pharmacological Basis of Therapeutics, McGraw-Hill, New York, 2001, pp. 1917-2024.
P. N. Jensen, O. V. Olesen, A. Bertelsen, and K. Linnet. Citalopram and desmethylcitalopram concentrations in breast milk and in serum of mother and infant. Ther. Drug Monit. 19:236-239 (1997).
O. Spigset, L. Carieborg, R. Ohman, and A. Norstrom. Excretion of citalopram in breast milk. Br. J. Clin. Pharmacol. 44:295-298 (1997).
K. E. Isenberg. Excretion of fluoxetine in human breast milk. J. Clin. Psychiatry 51:169(1990).
S. Wright, S. Dawling, and J. J. Ashford. Excretion of fluvoxamine in breast milk. Br. J. Clin. Pharmacol. 31:209(1991).
O. Spigset, L. Carleborg, A. Norstrom, and M. Sandlund. Paroxetine level in breast milk. J. Clin. Psychiatry 57:39(1996).
R. Ohman, S. Hagg, L. Carleborg, and O. Spigset. Excretion of paroxetine into breast milk. J. Clin. Psychiatry 60:519-523 (1999).
L. L. Altshuler, V. K. Burt, M. McMullen, and V. Hendrick. Breastfeeding and sertraline: a 24-hour analysis. J. Clin. Psychiatry 56:243-245 (1995).
K. F. Ilett, J. H. Kristensen, L. P. Hackett, M. Paech, R. Kohan. and J. Rampono. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br. J. Clin. Pharmacol. 53:17-22 (2002).
S. Rattigan, A. V. Ghisalberti, and P. E. Hartmann. Breast-milk production in Australian women. Br. J. Nutr. 45:243-249 (1981).
N. F. Butte, C. Garza, J. E. Stuff, E. O. Smith, and B. L. Nichols. Effect of maternal diet and body composition on lactational performance. Am. J. Clin. Nutr. 39:296-306 (1984).
M. C. Neville. Physiology of lactation. Clin. Perinatol. 26:251-279 (1999).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McNamara, P.J., Abbassi, M. Neonatal Exposure to Drugs in Breast Milk. Pharm Res 21, 555–566 (2004). https://doi.org/10.1023/B:PHAM.0000022401.14710.c5
Issue Date:
DOI: https://doi.org/10.1023/B:PHAM.0000022401.14710.c5