Abstract
Introduction and aims
The role of and optimal surgical revascularisation technique for paediatric moyamoya syndrome (MMS) are controversial. In this literature review our primary aim was to evaluate the evidence base for the efficacy of surgical revascularisation for the treatment of paediatric MMS. Secondary aims were to estimate the rate of peri-operative complications and to ascertain whether direct or indirect revascularisation techniques resulted in differences in clinical or radiological outcomes.
Methods
Papers describing surgical revascularisation and its outcome in the treatment of children with MMS were identified from the OVID Medline database (1966–2004). Only papers in English were reviewed. Data were abstracted using a standardised form.
Results
Fifty-seven studies, including data on 1,448 patients, were reviewed. Most were Japanese; 10% were from Western institutions. Indications for revascularisation were described in <15% of studies and varied between centres. Indirect procedures were most commonly performed (alone in 73% of cases, combined with direct procedures in 23%). The rates of peri-operative stroke and reversible ischaemic events were 4.4 and 6.1% respectively. Out of 1,156 (87%) patients, 1,003 derived symptomatic benefit from surgical revascularisation (complete disappearance or reduction in symptomatic cerebral ischaemia), with no significant difference between the indirect and direct/combined groups. Data on developmental and functional outcomes were limited and of uncertain significance as they were not related to pre-operative status. Good collateral formation was significantly more frequent in the direct/combined group than in the indirect group (χ2, p<0.001).
Conclusions
Data from the medical literature suggest that surgical revascularisation is a safe intervention for paediatric MMS and most treated patients derive some symptomatic benefit. However, paucity of data on selection criteria and more global outcome measures means that the impact of surgical revascularisation on natural history remains uncertain. Direct and/or combined procedures provide better revascularisation, but this is not associated with differences in symptomatic outcome. International standardisation of the clinical approach to the treatment of paediatric MMS is urgently needed to critically evaluate the optimal indications for and timing of surgical revascularisation.
Similar content being viewed by others
Introduction
Moyamoya syndrome is a radiological term describing a cerebral arteriopathy characterised by stenosis or occlusion of the terminal internal carotid (ICA) or anterior or middle cerebral arteries (ACA or MCA) with profuse lenticulostriate collaterals. Cases were initially reported in Japan where the prevalence is 3 in 100,000 [33]. It has subsequently been recognised worldwide, although remaining much more common in patients of Japanese and Asian ethnicity. The arteriopathy may be progressive [17].
Four main clinical presentations are recognised: with cerebral infarction, transient ischaemic attacks (TIA), cerebral haemorrhage and epileptic seizures. Ischaemic symptoms predominate in children. In addition to overt stroke or TIA, there may also be progressive decline in cognitive function [6], related to chronic cerebral hypoperfusion. The clinical consequences of moyamoya are significant, with a high incidence of recurrent stroke and TIA, and major neurological and cognitive impairments in many patients [2, 3, 13]. Young age of onset predicts a more aggressive clinical course [13]. However, there is a spectrum of outcomes and some patients are minimally affected. Small studies from the United States have suggested that outcomes may be more benign in non-Japanese patients [34]. At present it is not possible to reliably predict outcome in individual cases.
Several treatments have been considered for prevention of recurrent cerebral ischaemia. Medical treatments (for example, vasodilators, low molecular dextrans and steroids) are ineffective. A variety of surgical techniques have been developed, aimed at improving blood flow to the chronically hypoperfused brain. The first surgical treatment, cervical sympathectomy (performed to decrease vasomotor tone) [28], was ineffective in the long term [9]. Subsequently, a range of surgical techniques was developed to revascularise the ischaemic cerebral cortex. Many techniques have been described; they can be divided into direct procedures (involving direct anastomosis of arteries between the extracranial and intracranial circulations), and indirect procedures (in which the superficial temporal artery or vascularised tissues, such as the temporalis muscle, dura mater or omentum, are placed directly on the brain surface, to promote collateral formation).
The indications for, and timing of, surgical revascularisation in paediatric moyamoya are controversial, especially as the natural history is so variable [19, 24]. Direct arterial anastomosis is technically challenging in young children and it has been unclear whether it confers any specific advantage over the more straightforward indirect techniques. The primary aim of this paper is to review the English language literature to ascertain the efficacy of surgical revascularisation in the treatment of paediatric moyamoya syndrome. Secondary aims are firstly, to describe the rate of peri-operative complications and, secondly, to ascertain whether direct or indirect revascularisation techniques result in differences in clinical or radiological outcomes.
Materials and methods
The OVID MEDLINE database covering 1966–2004 was searched, using ‘moyamoya’ as the keyword to focus and explode. Inclusion criteria were papers that included:
-
1.
Data on surgical treatment of moyamoya
-
2.
Patients aged under 21 years
-
3.
Data on five or more patients
Studies that did not report the outcome of surgical treatment and publications in languages other than English were excluded from the review. A standard data extraction sheet was used to abstract the following data from the original papers:
-
1.
Demographic data (age, ethnicity, clinical presentation, secondary diagnoses, pre-operative status)
-
2.
Indications for surgery
-
3.
Interval between diagnosis and treatment
-
4.
Surgical technique
-
5.
Peri-operative complications
-
6.
Surgical outcome (clinical status, developmental progress, cognitive function, quality of life) and radiological outcome (angiography and cerebral perfusion parameters)
Where appropriate χ2 tests were used to compare complication rates and clinical and radiological outcomes between direct and indirect revascularisation groups.
Results
A total of 1,260 articles were identified (896 in English, 227 in Japanese). Fifty-nine met the inclusion criteria. Forty-eight of these were purely paediatric studies and the rest included both adults and children. Four studies came from the same patient database from two different centres. After excluding definitely overlapping studies, we analysed data from 57 studies, which included data from 1,448 patients, of whom 1,322 (91%) were under 21 years of age. All were retrospective case series. Forty-two (74%) of them came from Japanese institutions; 3 came from non-Japanese Asian countries, 7 from the USA, 3 from Canada and 1 each from Italy and the UK.
Demographic features and clinical presentation
The patients included in these studies had a wide age range at presentation, from 1 month to 59 years (mean 7.2 years). Twenty-two studies stated the ethnicity of the patients: 14 of them included 284 Japanese patients, the other 7 studies involved 211 Caucasian patients, 35 Asians, 9 black patients and 6 patients of other ethnicity. Only patients with idiopathic moyamoya “disease” were included in the Japanese studies, but patients with associated conditions were also included in many of the western studies. Among the 338 patients described in 12 western studies, 29 had neurofibromatosis type 1, 20 had a history of cranial irradiation, 16 had Down syndrome, 2 had renovascular hypertension and 47 had other diagnoses (Noonan syndrome, hypothyroidism, sickle cell disease and various congenital heart diseases). Diagnostic criteria were documented in only 6 studies, of which 3 had used the criteria from the Japanese Research Committee on Spontaneous Occlusion of the Circle of Willis of the Ministry of Health and Welfare. Pre-operative angiographic staging (using the Suzuki classification [27]) was only documented in 8 studies (479 patients). Patients with stage I and II disease accounted for 19.8%, stage III for 51.6%, stage IV for 24.8%, and stages V and VI for 3.7%.
Clinical features or presenting symptoms were described in 48 studies (84%). Over 80% of patients presented with ischaemic symptoms (TIA or cerebral infarction). Three hundred and fifty-three out of 1,084 patients (33%) for whom data regarding clinical presentation were available had radiological confirmation of cerebral infarction. Fifty-seven patients (5%) presented with epilepsy and 27 patients (2.5%) presented with intracranial haemorrhage. The remaining patients presented with headache, movement disorders or a mixture of symptoms. Pre-operative neurological status was described in only eight of the studies. Twenty-three out of 56 patients from three studies had persistent neurological deficits prior to surgery. Forty-four out of 117 patients (38%) from five studies had significant cognitive impairment (IQ or developmental quotient <80).
Indications for surgical revascularisation
Eight of the 55 studies (14.5%) described indications for surgical revascularisation. These were not always clearly described and were not consistent. Examples of indications stated include: “neurological signs and symptoms likely to be related to cerebral ischaemia and angiographic documentation of moyamoya disease” [20], “repeated ischaemic attacks or progressive mental retardation” [16], “low cerebral blood flow in the frontal or occipital area, frontal or occipital atrophy on CT” [30], “transient weakness or hypoperfusion” [7], “inexorable progression of symptoms” [21], “symptomatic/decreased haemodynamic reserve on cerebral blood flow study” [18], “recurrent TIA and/or stroke after first operation” [31] and “ischaemic” symptoms [32]. Thus, there was some variation in whether progressive or recurrent symptoms were required in order for surgical revascularisation to be considered. The mean interval between presentation and surgery was 23.8 months (range 0.5–168 months).
Surgical techniques
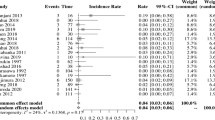
Of the 2,218 hemispheres treated, 92 were treated with direct procedures (4%), 1,618 (73%) with indirect procedures and 508 (23%) with combination of both direct and indirect procedures (see Fig. 1). There has been no standardised surgical approach and numerous surgical procedures have been used in a variety of combinations. The commonest direct revascularisation procedure used was anastomosis of the superficial temporal artery (STA) to the MCA, either in isolation or in combination with a variety of indirect procedures, e.g. encephaloarteriodurosynangiosis (EDAS), encephalomyosynangiosis (EMS), encephalo-duro-arterio-myosyangiosis (EDAMS), modified EDAS (pial synangiosis) [1], ribbon EDAMS [12], encephalo-galeo-synangiosis (EGS) [29], split duroencephalosynangiosis [10, 12], omental transfer [31] and gracilis muscle transfer [32]. Different combinations of indirect procedures have also been used in the same patient. The large number of indirect techniques or combinations of techniques precluded separate analysis; therefore, all indirect techniques have been considered as one group.
Post-surgical outcome and relationship to surgical technique
The duration of post-operative follow-up was 1 month to 19.5 years (mean 53.7 months). The surgical results are summarised in Table 1. Overall, 592 out of 1,156 previously symptomatic patients (51.2%) became completely asymptomatic (with disappearance of TIAs and no neurological signs), 411 (35.5%) had definite improvement (decreased frequency and/or severity of symptoms), 122 (10.5%) remained static (symptoms and/or neurological deficit persisted) and 31 (2.7%) had definite deterioration (including development of new infarcts). There was no significant difference in the rate of positive outcomes (asymptomatic or definite improvement) between the indirect and the direct/combined groups.
Data on developmental outcome were only available for 72 patients, of whom 20 (28%) improved, 38 (53%) were static and 14 (19%) deteriorated after surgery. Data on quality of life were available for 272 patients; 187 (69%) were independent, 64 (23%) were partially dependent in daily activities and the remaining 21 (8%) patients were totally dependent in daily activities. Unfortunately, no data regarding their pre-operative status were available for comparison and there were insufficient data to compare direct and indirect techniques.
Several studies reported post-operative angiographic results, either in qualitative terms (e.g. ‘good’ or ‘fair’ revascularisation) [30] or semi-quantitatively, as first described by Matsushima et al.—revascularisation of more than two-thirds, one-third to two-thirds, or less than one-third of the territories supplied by the MCA [14]. Post-operative angiography showed ‘good or significant’ collateral formation or at least revascularisation in one-third of the MCA territories after 719 out of 864 (83%) indirect procedures, 6 out of 7 direct procedures and 97 out of 101 combined procedures. Comparing the indirect group with pooled data from the direct and combined group, good collateral formation was significantly more frequent in the direct/combined group (χ2 test, p<0.01).
Eleven studies reported qualitative or semi-quantitative results of post-operative cerebral perfusion studies, either xenon computerised tomography (7 studies) or single photon emission computed tomography (SPECT). One hundred and ninety-three out of 290 (68%) patients were reported to have post-operative improvement of cerebral perfusion. There were insufficient data for comparing direct and indirect methods.
Peri-operative complications
Only 25 studies (686 patients) provided data on peri-operative complications, but often these were not described in relation to the specific procedures undertaken. The available data are summarised in Table 2. The rate of stroke and reversible cerebral ischaemic events (reversible ischaemic neurological deficit and TIA) related to revascularisation surgery was 4.4 and 6.1% respectively. Seizures, haemorrhage and infection were relatively uncommon. Some of the peri-operative complication rates were described in the surgical group as a whole, including different combinations of procedures, making further detailed analysis impossible.
Discussion
As moyamoya is common in Japan, much of the literature regarding treatment is in Japanese. However, more than three-quarters of the data in the English literature originates from Japan and the Japanese Research Committee on Spontaneous Occlusion of the Circle of Willis of the Ministry of Health and Welfare has summarised the current state of Japanese research in the English literature [4]. There is potential for overlap of the data included in this review as some of the studies came from the same institutions during overlapping periods. All the studies were heterogeneous in terms of evaluation protocols, making comparison between centres or objective evaluation of the interventions described extremely difficult. It is possible that more studies with positive rather than negative results would have been submitted for publication, introducing another potential source of bias in the data available for this review. The western studies included patients with secondary causes of moyamoya, such as Down syndrome or neurofibromatosis 1. However, there were no data on whether these co-existing conditions influence natural history and therefore the treatment approach.
One of the main difficulties in evaluating the efficacy of revascularisation is the limited data on natural history, and on the factors determining this. Although absence of recurrence could be deemed a successful outcome of surgery, this is only meaningful if compared with the rate of expected deterioration in untreated patients. From the limited pre-operative data reported it is apparent that a large number of patients already have fixed impairments at the time of surgery. Thus, clinical evaluation alone may be an inadequate measure of the efficacy of surgery as such impairments are unlikely to be altered; additional parameters that should be considered include cognitive status, functional and quality of life measures, as well as radiological evaluation to exclude silent re-infarction and to detect improvements in cerebral perfusion or haemodynamic reserve. One effect of the uncertainty regarding the role of surgery, and the present inability to identify patients at high risk of deterioration at presentation, is that there is often a significant delay between diagnosis and treatment (a mean of 2 years in the studies reviewed).
The predominance of indirect procedures reflects the relative difficulty of direct revascularisation in young children. However, a great variety of techniques are in use and their relative efficacy is difficult to evaluate. Although angiographic studies provide an objective measure of revascularisation, the correlation with clinical status is unclear. The patency of direct revascularisation can be established soon after the operation [22], but in indirect procedures collaterals may take at least 6 months to develop [15]. From the pooled results, direct and/or combined surgical methods were associated with significantly better revascularisation. There were no significant differences in outcome between the two groups, although this was a conservative analysis as patients with a static clinical course may potentially also have benefited from surgery by having no further progression of disease. Ikezaki reported a nationwide survey in Japan that included 651 paediatric patients [5]. He found that 38.3% of unoperated patients required surgery eventually. For the groups with direct bypass surgery, indirect bypass surgery and combined direct and indirect surgery, the rates of re-operation were 2.8, 18 and 1.8% respectively. Thus, a significant number of patients managed conservatively were subsequently treated with surgery and secondary operations were less commonly required in patients who had had direct procedures. However, these data are difficult to interpret as the factors underlying both the initial and subsequent treatment decisions were not stated.
The description of surgical results was very variable and different ‘classification systems’ have been used to describe outcome [11, 12]. One thousand and three of the 1,156 patients (86.8%) had definite improvement in their symptoms and only 2.3% showed definite clinical progression after surgery. This contrasts with the high rate of poor outcome or progressive symptoms reported in several natural history studies, in the region of 50–66% [2, 3, 13]. Scott et al. reported the largest series of surgical revascularisation in MMS in the western hemisphere. Describing the results of their series of indirect procedures they conclude that ‘surgery halts what is normally a relentless clinical deterioration in the untreated patient’ [25].
The quality of the evidence summarised in this review is relatively poor (Grade 3 according to the Scottish Intercollegiate Guidelines Network [SIGN] grading scheme) and therefore surgical revascularisation is a treatment that constitutes a grade D recommendation (see Table 3 for levels of evidence and recommendations) [26]. Fukui [4] reported that in 821 patients registered in Japan up to 1994 there were no significant differences between medically and surgically treated patients. Selection bias is an important consideration, as this review confirms that in many centres surgical treatment is offered to patients with recurrent or progressive symptoms. The guidelines for diagnosis and treatment of moyamoya disease from the Committee on Moyamoya Disease of the Ministry of Health and Welfare of Japan advise surgical treatment for patients with repeated clinical symptoms due to apparent cerebral ischaemia or decreased regional cerebral blood flow, vascular response and perfusion reserve, based on the findings of a cerebral circulation and metabolism study. However, as the results of cerebral blood flow or metabolism studies were only rarely reported in the literature, it is difficult to comment on the consistency of the clinical approach between centres. Although there are data to suggest that patients presenting in childhood have a more aggressive clinical course [3, 5, 13], it is uncertain whether similar surgical indications should apply to children and adults.
Potential complications of surgical revascularisation are likely to relate to anaesthetic factors as well as to surgical technique [8, 23], but overall the rate is relatively low. The optimal surgical techniques will be limited by technical feasibility as well as relative efficacy. One approach, proposed by Ikezaki, is to use combined direct and indirect procedures in children aged over 8 years, with adequate recipient and donor arteries, and those in need of urgent intervention because of recurrent TIAs, and to undertake indirect techniques in children younger than 8 years [5]. The feasibility and efficacy of such an approach could be prospectively evaluated if standardised evaluation protocols were developed and implemented across different centres. The weight of anecdotal evidence supporting the use of surgical revascularisation in the treatment of paediatric moyamoya means that a randomised controlled trial is unlikely to prove acceptable to affected children and their families. This reinforces the need for international consensus on peri-operative assessment and treatment so that future clinical practice can be standardised and prospectively evaluated.
References
Adelson PD, Scott RM (1995) Pial synangiosis for moyamoya syndrome in children. Pediatr Neurosurg 23:26–33
Choi JU, Kim DS, Kim EY, Lee KC (1997) Natural history of moyamoya disease: comparison of activity of daily living in surgery and non surgery groups. Clin Neurol Neurosurg 99 [Suppl 2]:S11–S18
Ezura M, Yoshimoto T, Fujiwara S, Takahashi A, Shirane R, Mizoi K (1995) Clinical and angiographic follow-up of childhood-onset moyamoya disease. Childs Nerv Syst 11:591–594
Fukui M (1997) Current state of study on moyamoya disease in Japan. Surg Neurol 47:138–143
Ikezaki K (2000) Rational approach to treatment of moyamoya disease in childhood. J Child Neurol 15:350–356
Imaizumi C, Imaizumi T, Osawa M, Fukuyama Y, Takeshita M (1999) Serial intelligence test scores in pediatric moyamoya disease. Neuropediatrics 30:294–299
Iwama T, Hashimoto N, Tsukahara T, Miyake H (1997) Superficial temporal artery to anterior cerebral artery direct anastomosis in patients with moyamoya disease. Clin Neurol Neurosurg 99 [Suppl 2]:S134–S136
Kansha M, Irita K, Takahashi S, Matsushima T (1997) Anesthetic management of children with moyamoya disease. Clin Neurol Neurosurg 99 [Suppl 2]:S110–S113
Karasawa J, Kikuchi H, Furuse S, Kawamura J, Sakaki T (1978) Treatment of moyamoya disease with STA-MCA anastomosis. J Neurosurg 49:679–688
Kashiwagi S, Kato S, Yasuhara S, Wakuta Y, Yamashita T, Ito H (1996) Use of a split dura for revascularization of ischemic hemispheres in moyamoya disease. J Neurosurg 85:380–383
Kim SK, Wang KC, Kim IO, Lee DS, Cho BK (2002) Combined encephaloduroarteriosynangiosis and bifrontal encephalogaleo(periosteal)synangiosis in pediatric moyamoya disease. Neurosurgery 50:88–96
Kinugasa K, Mandai S, Tokunaga K, Kamata I, Sugiu K, Handa A, Ohmoto T (1994) Ribbon enchephalo-duro-arterio-myo-synangiosis for moyamoya disease. Surg Neurol 41:455–461
Kurokawa T, Tomita S, Ueda K, Narazaki O, Hanai T, Hasuo K, Matsushima T, Kitamura K (1985) Prognosis of occlusive disease of the circle of Willis (moyamoya disease) in children. Pediatr Neurol 1:274–277
Matsushima T, Inoue T, Suzuki SO, Fujii K, Fukui M, Hasuo K (1992) Surgical treatment of moyamoya disease in pediatric patients—comparison between the results of indirect and direct revascularization procedures. Neurosurgery 31:401–405
Matsushima Y, Inaba Y (1984) Moyamoya disease in children and its surgical treatment. Introduction of a new surgical procedure and its follow-up angiograms. Childs Brain 11:155–170
Miyamoto S, Nagata I, Hashimoto N, Kikuchi H (1998) Direct anastomotic bypass for cerebrovascular moyamoya disease. Neurol Med Chir (Tokyo) 38 [Suppl]:294–296
Murphy MJ (1980) Progressive vascular changes in Moyamoya syndrome. Stroke 11:656–658
Nakashima H, Meguro T, Kawada S, Hirotsune N, Ohmoto T (1997) Long-term results of surgically treated moyamoya disease. Clin Neurol Neurosurg 99 [Suppl 2]:S156–S161
Roach ES (2001) Immediate surgery for moyamoya syndrome? Not necessarily. Arch Neurol 58:130–131
Robertson RL, Burrows PE, Barnes PD, Robson CD, Poussaint TY, Scott RM (1997) Angiographic changes after pial synangiosis in childhood moyamoya disease. Am J Neuroradiol 18:837–845
Rooney CM, Kaye EM, Scott RM, Klucznik RP, Rosman NP (1991) Modified encephaloduroarteriosynangiosis as a surgical treatment of childhood moyamoya disease: report of five cases. J Child Neurol 6:24–31
Sakamoto H, Kitano S, Yasui T, Komiyama M, Nishikawa M, Iwai Y, Yamanaka K, Nakajima H, Kishi H, Kan M, Fujitani K, Hakuba A (1997) Direct extracranial–intracranial bypass for children with moyamoya disease. Clin Neurol Neurosurg 99 [Suppl 2]:S128–S133
Sato K, Shirane R, Yoshimoto T (1997) Perioperative factors related to the development of ischemic complications in patients with moyamoya disease. Childs Nerv Syst 13:68–72
Scott RM (2001) Surgery for moyamoya syndrome? Yes. Arch Neurol 58:128–129
Scott RM, Smith JL, Robertson RL, Madsen JR, Sorian SG (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg 100 [Suppl 2]:142–149
Scottish Intercollegiate Guidelines Network. Available at http://www.sign.ac.uk
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Suzuki J, Takaku A, Kodama N, Sato S (1975) An attempt to treat cerebrovascular ‘Moyamoya’ disease in children. Childs Brain 1:193–206
Takikawa S, Kamiyama H, Abe H, Mitsumori K, Tsuru M (1990) Hemodynamic evaluation of vascular reconstructive surgery for childhood moyamoya disease using single photon emission computed tomography. Neurol Med Chir (Tokyo) 30:389–395
Tenjin H, Ueda S (1997) Multiple EDAS (encephalo-duro-arterio-synangiosis). Additional EDAS using the frontal branch of the superficial temporal artery (STA) and the occipital artery for pediatric moyamoya patients in whom EDAS using the parietal branch of STA was insufficient. Childs Nerv Syst 13:220–224
Touho H, Karasawa J, Ohnishi H, Yamada K, Shibamoto K (1993) Surgical reconstruction of failed indirect anastomosis in childhood Moyamoya disease. Neurosurgery 32:935–940
Touho H, Karasawa J, Ohnishi H (1995) Cerebral revascularization using gracilis muscle transplantation for childhood moyamoya disease. Surg Neurol 43:191–197
Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, Kojima M, Lin Y, Ohno Y (1997) Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg 99 [Suppl 2]:S1–S5
Yilmaz EY, Pritz MB, Bruno A, Lopez-Yunez A, Biller J (2001) Moyamoya: Indiana University Medical Center experience. Arch Neurol 58:1274–1278
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fung, LW.E., Thompson, D. & Ganesan, V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Childs Nerv Syst 21, 358–364 (2005). https://doi.org/10.1007/s00381-004-1118-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-004-1118-9